
Board of Directors Meeting
Meeting in public to be held on 23rd November 2023 at 12.30 via MS Teams
AGENDA
D – for discussion, A – for approval/decision, Ac – Action
|
Time |
Item |
Item |
Presenter |
Action |
Paper/ Verbal |
|---|---|---|---|---|---|
12.30 | 23.53 | Chair’s welcome, apologies for absence and notification of any urgent business: Pip Coker, Jason Hollidge | Zoë Billingham | Verbal | |
12.32 | 23.54 | Declarations of Interest | Zoë Billingham | D | Paper A |
12.33 | 23.55 | To approve the minutes of the previous public meeting, held on 28th September 2023 | Zoë Billingham | A | Paper B |
12.35 | 23.56 | To address any Matters Arising from the minutes of the previous meeting and Action Log | Zoë Billingham | Ac | Paper C |
12.45 | 23.57 |
| Zoë Billingham Caroline Donavan Kimberly Gillingham Lindsey Hoy | D D D A | |
Exceptional Care | |||||
13.10 | 23.58 |
| Ac D D D I I I | ||
Roger Hall Tumi Banda Alex Lewis Tumi Banda Tumi Banda Alex Lewis | |||||
14.05 | 23.59 | Performance and Finance Committee Chair’s report
| Adrian Matthews Thandie Matambanadzo Kathy Walsh | D D D A | |
Transforming Lives | |||||
14.25 | 23.60 | Strategy and Improvement programme Report | Kathryn Ellis | I | Paper O |
Inspirational People | |||||
14.35 | 23.61 |
| Tricia Fuller Cath Byford | D D | |
Questions from the Public |
The Board of NSFT sets the strategic direction, vision and purpose of the organisation and establishes the culture and values. The board oversees delivery of strategic objectives, seeking assurance that risks to the organisation are mitigated and ensuring value for money. Led by an independent chair and composed of both executive and independent non-executive members, the Trust board has a collective responsibility for ensuring high quality safe and effective services for our service users, carers and our local community.
|
Date: 23rd November 2023 |
A |
|---|---|
|
Item: 23.54 |
Board of Directors Declaration of Interests: November 2023
We commit to openness and transparency in our work and decision making. As part of that commitment, we maintain and publish this register. The register draws together Declaration of Interests made by members of the Board of Directors.
Also, at the commencement of each Board meeting, we ask members of the Board to declare any interests on items on the agenda.
|
First Name |
Last name |
Position |
Details of interest |
|---|---|---|---|
Zoe | Billingham | Chair | Sole Director of Indigo Flame Limited. Freehold interest in 2 family homes together with my husband Trustee of SafeLives (a national domestic abuse charity) Member of the Aldeburgh Carnival Committee and a GoodSam NHS Volunteer Chair of the Police Pay Review Bodies and a NED on the Security Industry Authority (remunerated) Member of the Angiolini Inquiry Reference Group (unremunerated) Member of Labour Party Remunerated position of Specialist Advisor IPSOS Qualified Chair for the Pilot Programme of Offensive Weapons Homicide Reviews appointed by the Home Office (as required, remunerated) |
James | Barnard | Non Executive Director | Director/CIO Aviva (remunerated) Director Lenwade Mill Management - Residential Estate Management Holding (not remunerated) |
Pip | Coker | Non Executive Director | Previous role as CE of Julian Support Limited with whom the Trust has a contracting relationship. |
|
Tricia |
Fuller |
Non Executive Director |
Nil |
|---|---|---|---|
Roger | Hall | Clinical Non Executive Director | Director and shareholder of Cluroe and Hall Limited, a medical services company. I am inactive and member of the family provides private medical services (Remunerated) |
Sally | Hardy | Non Executive Director | Deliver annual Clinical Nursing Scholarships on behalf of the Worshipful Company of Barbers Academic Professor of Mental health and Practice Innovation at University of East Anglia (remunerated) Director of the Norfolk Initiative for Coastal and rural Health Equalities (NICHE), Anchor Institute, UEA (remunerated) |
Lindsey | Hoy | Non Executive Director | Family members have used limited services of the trust in the last 3 years. Executive Director at the London QEII Convention Centre & Chair of Audit and Risk Committee (remunerated) Non Executive Director at the East Coast Community Health Community Interest Company and Chair of Audit and Risk Committee (remunerated) |
Adrian | Matthews | Non Executive Director | Owner - XE Associates Consulting (Remunerated) National Job Evaluation Trainer - NHS Employers (Remunerated) Director - Diversa Trading Ltd. (unremunerated) Audit Committee Member - Norfolk Police & Crime Commission & Norfolk Constabulary (Remunerated) |
Caroline | Donovan | Interim Chief Executive | Director of CMD Health, providing leadership consultancy |
Cath | Byford | Deputy Chief Executive and Chief People Person | Nil |
Tumi | Banda | Interim Chief Nurse | Jabali Me’s Network |
|
Kathryn |
Ellis |
Chief Strategy, Improvement and Partnerships Officer |
Nil |
|---|---|---|---|
Jason | Hollidge | Chief Finance Officer | Close personal friend of Partner in Grant Thornton LLP Partner is a probation officer working for the Ministry of Justice and on occassion some of the offenders that she managers are in our inpatient units. |
Thandie | Matambanadzo | Chief Operating Officer | Nil |
Alex | Lewis | Interim Chief Medical Officer | Director of Quellwood Ltd (remunerated) Provides advisory work in healthcare. Member of NHS IMAS |
Unconfirmed minutes of the Board of Directors – Public Session
held on Thursday 28th September 2023, 1230, via MS Teams
|
Board of Directors |
Zoë Billingham (ZB) |
Chair |
|---|---|---|
Tricia Fuller (TF) | Non-Executive Director | |
Adrian Matthews (AM) | Non-Executive Director | |
James Barnard (JB) | Non-Executive Director | |
Pip Coker (PC) | Non-Executive Director | |
Sally Hardy (SH) | Non-Executive Director | |
Roger Hall (RH) | Non-Executive Director | |
Kathryn Ellis (KE) | Chief Strategy, Improvement and Partnerships Officer | |
Tumi Bandi (TB) | Interim Chief Nurse | |
Alex Lewis (AL) | Interim Chief Medical Officer | |
Jason Hollidge (JH) | Chief Finance Officer | |
Cath Byford (CB) | Deputy Chief Executive and Chief People Officer | |
Attendees: | Jean Clark (JC) | Trust Secretary |
April Brown (AB) | NHSE Improvement Director | |
Nicky Southgate (NS) | Corporate Governance Manager (minutes) |
5 staff, 4 members of the public, 9 governors The meeting started at. 12.30
|
Item |
Agenda title |
Action |
|---|---|---|
| 23.43 | Chair’s welcome, notification of any urgent business and apologies for absence | |
a) | Apologies were given by Lindsey Hoy, Stuart Richardson, Thandie Matambanadzo. | |
b) | ZB explained that Stuart Richardson, CEO, would be leaving the Trust at the end of October. ZB gave thanks and paid tribute to Stuart who had demonstrated kind and compassionate leadership and had led improvements in the Trust. The Trust were seeking to appoint an interim CEO and an announcement would be made as soon as possible. ZB thanked the Executive team for their exemplary leadership through this transition period. | |
| 23.44 | Declarations of Interest | |
a) | The declarations were NOTED. | |
| 23.45 | Minutes of the previous meeting | |
a) | The minutes of the meeting held on the 27th July 2023 were APPROVED as an accurate record with the correction of spelling mistakes. | |
| 23.46 | Matters arising and action log | |
| a) | The Board agreed to close the proposed actions and NOTED the action log updates. | |
| 23.47 | Chair and Chief Executive Report | |
a) | ZB introduced the report flagging the Annual General Meeting and Annual Members meeting on 7th November 2023 at the Mix, Stowmarket showcasing the work of the Trust. Medical leadership and engagement had been enhanced with a range of |
|
Item |
Agenda title |
Action |
|---|---|---|
actions being taken forward and the board was meeting regularly with the Medical Staffing Committee; ZB thanked AL and colleagues for progress. | ||
| b) | ZB reminded that the governor nomination period would be open from 16th October to 31st October 2023 and this year there were vacancies for two carer governors, four public governors and three staff governors. Governors were holding information events for those interested. All details were available on the website. | |
| c) | CB presented the CEO report and commended colleagues during period of industrial action, and thanked the Resilience team and Tactical Commanders, Richard Green and Dawn Collins. | |
Response to Letby issues | ||
| d) | CB introduced the report explaining the Trust’s approach was wider than the letter received from NHS England, encouraging staff to raise concerns through a range of mechanisms in addition to Freedom to Speak Up (FTSU). The culture change programme was fundamental, and a multidisciplinary approach was needed to resolving issues. | |
| e) | TF explained the People and Remuneration Committee had discussed the response at length and noted that there was more work required to understand the reasons staff used the service and more resource needed to support the FTSU Guardian. | |
| f) | The Board agreed this paper was only part of the picture and asked CB to consider how the board continues to reflect on addressing these issues and address the support for the FTSU Guardian. Action | CB |
| g) | PC was pleased to see this was not just about FTSU and asked how supervision was used to raise issues. CB agreed supervision was one of key mechanisms people should be able to raise issues and referred to a question raised by a member of the public in regard supervision being high quality and impactful. The data suggests people go to FTSU because they have not been listened to by their manager, so efforts were focusing on developing capable and confident managers through leadership programmes and a leadership competency framework. | |
| h) | The Board NOTED the report. | |
Freedom to Speak Up Report | ||
Ade Adetukasi (AA) joined for this item. | ||
| i) | AA presented the report as the FTSU guardian was unable to attend and drew the Boards attention to the improving data quality and reiterated that the resource issue needed to be resolved. JH added that it was essential the service remained confidential; we welcome staff identifying themselves but the action taken on concerns was the same regardless. | |
| j) | The Board were pleased that more people were speaking up with the FTSU Guardian. |
|
Item |
Agenda title |
Action |
|---|---|---|
| k) | TB asked how the Trust was ensuring it recruited competent managers. CB responded there was still work to be done. | |
| l) | The Board NOTED the report. | |
Audit and Risk Committee Chair’s report | ||
| m) | AM presented the report in LH absence and highlighted the Emergency Response and Resilience Team who were carrying out great work behind the scenes ensuring the Trust was ready for emergency situations. | |
| n) | AM noted the temporary access card issue which the Information Governance team were looking at and will report back at the next meeting. Action. PC noted this was a good example of balancing risk appetite and mitigating unintended consequences of addressing another risk. | JH |
| o) | The Board NOTED the report. | |
| 23.48 | People and Remuneration Committee Chair’s Report | |
| a) | TF presented the Chair’s report and highlighted the committee’s concern with recruitment retention supervision and appraisal. TF noted that many of the staff leaving within two years were administration staff and a programme to support career development was needed with a dedicated lead. CB agreed executive leadership was needed. ACTION. AM offered support in his role as NED sponsor for the Administration network. | CB |
| b) | The Board requested a future update on the framework being used for exit interviews. ACTION | CB |
| c) | The Board NOTED the report. | |
Workforce Performance | ||
| d) | CB highlighted key points from the report. | |
Guardian of Safe Working | ||
Kapil Bakshi (KB) joined for this item | ||
| e) | KB introduced the report explaining that all junior doctors have a contract and rotas are compliant. There had been five exemption reports in the reporting period which was within the norm and none were related to patient safety incidents or loss of educational opportunities. There was one incident where one individual had been discouraging junior doctors not to raise incidents – the individual had been spoken to, and had attended the junior doctor forum to reiterate the contractual requirement to report. KB commended the medical HR team arranging cover during the industrial action. | |
| f) | The Board thanked KB and the medical HR team and reinforced the absolute requirement of reporting all incidents. JH added that there were checks in that area and can confirm a positive reporting culture now. KB has reminded trainees to approach him for any support. |
|
Item |
Agenda title |
Action |
|---|---|---|
| g) | The Board noted the report. | |
Annual statement of Compliance for responsible officers (RO) and revalidation | ||
Jan Falkowski joined for this item | ||
| h) | JF presented the report as he had recently taken on the role from Dr Dan Dalton. JF would provide the People and Remuneration Committee with regular updates and was establishing a Responsible Officer Advisory group to review revalidation evidence. | |
| i) | KE questioned how the quality of appraisals and supervision were measured and evidenced. JF explained data was gathered from the appraisee via the Allocate system but without the appraiser knowing, so additional data was gathered. | |
| j) | RH commended the high appraisal rates. | |
| k) | The Board APPROVED the RO annual statement of compliance for responsible officers and revalidation, noted JF’s appointment as RO and thanked Dr Dalton. | |
| 23.49 | Quality Assurance Committee Chairs report | |
a) | RH presented his Chair’s report escalating concerns regarding timely recruitment and the need for a system wide response to the physical health needs of service users. | |
b) | TB confirmed the two posts to support the quality and safety pillar were now out to advert and explained the quality of the job descriptions had meant delay with the Fair Recruitment Panel. CB added that the issue was dealt with as soon as it was raised and it was the check and challenge prior to being seen at panel that caused the delay. | |
c) | The Board NOTED the report. | |
Quality and Safety Performance | ||
d) | TB presented the quality and safety performance and highlighted the work on managing and preventing serious incidents. Safe wards programme had been implemented and it was thought there was a correlation with this and reduction in seclusion and assaults on staff incidents. There had also been a reduction in the outstanding complaints also thought to be due to the quality improvement measures introduced. | |
e) | The Board NOTED the report. | |
Actions taken following Grant Thornton review and ‘Forever Gone’ report | ||
f) | ZB introduced the reports emphasising that rapid improvements were required to address the issues raised in the Grant Thornton review. CB reminded Board that the authors of ‘Forever Gone’ had joined the July Board to present their response to the review. The Board remained committed to working with them, other bereaved families, service users and carers and partners in a co-produced way and had agreed clear commitments: agreeing a dataset in a way that humanises the data; |
|
Item |
Agenda title |
Action |
|---|---|---|
building on the bereavement project work to support bereaved families and better learning from deaths, and with system partners tackling health inequalities to prevent people with mental health from dying early. The Board had committed to being a restless curious board. | ||
g) | AL explained the progress being made on the Grant Thornton action plan. ZB confirmed the status of the action plan ensuring all the elements of co-production were added. AL explained that there had been discussions with all partners and service users and carers and many actions were underway. | |
h) | TB reiterated the commitment to listen to and learn from bereaved families and noted the work since July, coproducing learning summits, engagement strategy and upskilling the workforce to better support families. The Trust was recruiting two Family Liaison Officers and it was hoped this would be expanded with system partners. TB thanked all the families who had shared their experiences to help us develop the work. | |
i) | AM asked what support was being provided to the bereaved families involved as this was a difficult thing to do. TB confirmed the families who had been involved were offered support by himself and the Head of Carer and Head of Service User Experience. | |
j) | AM noted the three elements to the work and asked about work to reduce the life expectancy gap for those with serious mental illness (SMI). AL explained this was a national gap and required a whole system approach with the Integrated Care Partnerships, primary care and public health. | |
k) | ZB reflected that the report had galvanised the support of Integrated Care Board colleagues and for them to reconsider how mental health is prioritised. CB commented on the recent event with Healthwatch Norfolk, seeing through the lens of families of those with a serious mental illness. System partners were being asked to come together to wrap around support with, for example, social care and housing. There was now a specific risk on the Board Assurance Framework to monitor the actions being taken. | |
l) | The Board NOTED the report. | |
23.50 | Performance and Finance Committee Chair’s report | |
a) | AM presented the report and highlighted the sustained improvement in the eating disorder service. The fragile system finance position was concerning and needed to be kept under review. NEDs had commissioned a deep dive in to the waiting lists for Norfolk and Waveney Children, Family and Young People services because whilst a lot of work was being done to reduce the waiting times, the improvements were not as visible as expected. | |
b) | ZB encouraged looking at the wider picture, and review if resources were organised with the right balance between community and inpatients. | |
c) | CB noted the revised Board Assurance Framework (BAF), following its annual review, describing the key risks to delivering the new Trust Strategy, with many risks |
|
Item |
Agenda title |
Action |
|---|---|---|
carried over from last year and new risks raised. The BAF was discussed in detail by each Board committee. | ||
d) | KE commented about the scope of efficiencies. There was active work to improvement activities, quality improvement alongside discussions on the effective use of resources to continue the improvement journey. Dialogue with the wider system as part of our annual planning process provided natural opportunities to engage with system colleagues to plan for future years investment. | |
e) | The Board NOTED the report. | |
Operational Performance | ||
f) | JH introduced the report for TM highlighting the favourable performance of Talking Therapies and Early Intervention in Psychosis team. There was challenging performance in crisis services and on planned care waiting lists. Referrals remained stable although benchmarking data continued to suggest NSFT were tracking above average and this was being investigated with the benchmarking network. | |
g) | TB asked for an update on the recording of physical health checks on Lorenzo, the electronic patient record. JH would check. ACTION | JH |
h) | KE was encouraged by the improving Talking Therapies performance. Having recently attended recently national Talking Therapies conference it was good to hear NSFT’s performance. The Board asked to formally thank the Talking Therapy team. ACTION | JH |
i) | The Board NOTED the report. | |
Emergency Planning Annual Report | ||
j) | TB presented the report for TM which outlined compliance to the NHSE framework and associated core standards for emergency preparedness resilience and response. | |
k) | ZB asked for the Audit and Risk Committee to seek greater clarity in securing compliance for those areas highlighted in Annex 2. AM responded that this was already in train, although the availability of loggists was an issue for the whole system. | |
l) | The Board NOTED the report. | |
Finance and Use of Resources | ||
m) | JH explained the year to date financial position and forecast outturn, with reference to the BAF risk. Meetings were taking place with managers to gain traction with non recurrent plans. | |
n) | The Board NOTED the report. | |
Annual reports and accounts 2022-2023 |
|
Item |
Agenda title |
Action |
|---|---|---|
o) | JH presented the annual report and accounts 2022-2023 which had been laid in parliament and would be presented at the Annual General Meeting on 7th November 2023. | |
p) | The Board NOTED the report. | |
23.51 | Strategic update, improvement programme and system working | |
a) | The Board requested sufficient time was allowed for this item, Finance and Operational Performance at the next Board meeting. ACTION | JC |
b) | KE introduced the update describing it as a springboard that plans year on year, helping to demonstrate improvement, but critically to service users and staff. The strategy was monitored at the Improvement Board, Evidence Assurance Group and through the Recovery Support Programme. | |
c) | The Board NOTED the report. | |
23.52 | Questions from the Public in relation to the Board papers presented at today’s meeting are posted on the website along with responses. | |
a) | Date, time and location of next meeting | |
The next meeting of the Board of Directors in public will be held on the 23rd November 2023. | ||
Motion to exclude the public and press from the confidential part of the meeting to be held on the 23rd November 2023. |
There being no other business, the Chair thanked those present for their contribution and closed the meeting at 15.07.
Chair: Date:
Board of Directors – Action log – November 2023
|
Agenda item number |
Date |
Item |
Action |
Action by |
Due Date |
Status / Comments |
Date closed |
|---|---|---|---|---|---|---|---|
22.57f | 24/11/22 | IQPR - Performance | To update the board via the Performance and Finance Committee on the criteria for use of supported accommodation and on the data regarding physical health checks for people in specialist placements | Thandie Matambanadzo Tumi Banda | Nov 2023 | Supported accommodation discussed at May Performance and Finance Committee. Physical Health check work part of quality & safety pillar. | |
23.15g | 06/04/23 | Freedom to speak up | To present per capita data in future reports to better understand the data. | Kimberly Gillingham | Nov 2023 | Improved data reporting without identifying individuals | 23/11/23 |
23.18d | 06/04/23 | Workforce performance | To benchmark leavers data with other mental health trusts and report progress at each board meeting | Cath Byford | Nov 2023 | Power BI and Data Warehouse in development which will include benchmarking with local system providers. Wider work in progress to source reliable data with other MH providers (Model Hospital data will not meet this requirement). Propose to close this action on the Board log and monitor progress with the action at People and Culture Committee. | 23/11/23 |
23.19b. | 06/04/23 | Mental health collaboratives | To track progress with the developing governance of mental health collaboratives at future board | Kathryn Ellis | Nov 2023 | Full report on November Board | 23/11/23 |
|
Agenda item number |
Date |
Item |
Action |
Action by |
Due Date |
Status / Comments |
Date closed |
|---|---|---|---|---|---|---|---|
meetings | |||||||
23.28d. | 25/05/23 | People and Remuneration Chair report | To update Board on tangible actions being taken to address racism, pockets of poor culture | Cath Byford | November 2023 | “Launch and Learn” development programme introduced September 2023. Other initiatives include the fair recruitment panel and updating the Equality Diversity Inclusion strategy. Culture report regularly discussed at People & Culture Committee. Second Lunch and Learn session held, with both sessions having high engagement and participation – 309 people signed up to the programme (target was 250). Progress on the development of the People and Culture Strategy with progress reporting to the Board Committee in November. Propose to close this action on the Board log and monitor progress with the action at People and Culture Committee. | 23/11/23 |
23.28h. | 25/05/23 | Staff Survey | To update Board on progress with | Cath Byford | November | This is contained within the | 23/11/23 |
|
Agenda item number |
Date |
Item |
Action |
Action by |
Due Date |
Status / Comments |
Date closed |
|---|---|---|---|---|---|---|---|
Report | action plan for staff survey and broader culture work | Harprit Hockley | 2023 | draft People and Culture Strategy alongside the findings from the Big Conversation, WRES & WDES reports and Service User feedback. Specific updates following the ‘you said, we did’ principles reported to the People and Culture Forum (previous People Committee) and cascaded throughout the organisation through the Culture Change Agents (93 people), Health and Wellbeing Champions (180 people), HR Business Partnering Team and the People and Culture Strategy Community of Improvement (450 people). Currently working with Comms to further widen trust- wide communication | |||
23.29e. | 25/05/23 | Service user experience | To meet with Norfolk CFYP regarding a blended approach to delivering services and service user expectations. | Thandie Matambanadzo | Nov 2023 | Part of Norfolk CFYP work – deep dive in progress |
|
Agenda item number |
Date |
Item |
Action |
Action by |
Due Date |
Status / Comments |
Date closed |
|---|---|---|---|---|---|---|---|
23.37c | 27/07/23 | Chair and Chief Executive Report | To update on the progress of opening all beds on Rollesby ward. | Thandie Matambanadzo | Nov 2023 | Providing status report to November board | |
23.37d | 27/07/23 | Chair and Chief Executive Report | To discuss the financial constraints on the Trust, ICBs and nationally and the importance of ensuring mental health received sufficient funding and support, with particular focus on prevention | Zoë Billingham | November 2023 | Continued lobbying at national and system meetings | |
23.37g | 27/07/23 | Freedom to Speak Up Report | To update on the progress of actions from the Freedom to Speak Up plan. | Cath Byford | September 2023 | Update provided at the September meeting. | 28/09/23 |
23.42n | 27/07/23 | Grant Thornton audit of mortality data reporting and response | For TM to meet with CA, AH, TB and AL to discuss the actions being taken. | Thandie Matambanadzo, Alex Lewis, Tumi Banda | September 2023 | Update provided at September meeting. Meeting had taken place and proposals for the way forward agreed. | 28/09/23 |
23.43m | 27/07/23 | Comments from members of the public | To reflect on next steps with CA and AH. | Zoë Billingham | September 2023 | An update as provided at the September meeting. | 28/09/23 |
23.47f | 28/09/23 | Response to Letby | To address the resource issues within the Freedom to Speak Up service. | Cath Byford | November 2023 | Agreement at Board for additional resource. PAC Team working with the Safety Teams a working group has |
|
Agenda item number |
Date |
Item |
Action |
Action by |
Due Date |
Status / Comments |
Date closed |
|---|---|---|---|---|---|---|---|
been set up and a proposal being taken to Senior Leadership Team. Decision made to extend the contract with the Guardian Service which included an options appraisal. F2SU policy updated in line with the National Guardians Office and NHS England. Whilst progressing additional capacity to address concerns, additional support given to the Guardian from the People and Culture Team. | |||||||
23.47n | 28/09/23 | Audit and Risk Committee Chair’s report | To update Board on how the matters relating to the use of Temporary Access Cards would be resolved. | Jason Hollidge | November 2023 | Raised issue at SLT to remind teams of the importance and discussed at November Audit & Risk Committee. Follow up audit carried resulting in directives to operational team managers. Executive will continue to monitor. | |
23.48a | 28/09/23 | People and Remuneration Committee Chair’s | To identify an Executive Lead for leading the admin review work | Cath Byford | November 2023 | The Medical Directorate leading interim arrangement and have identified additional resource for areas of urgency | 23/11/23 |
|
Agenda item number |
Date |
Item |
Action |
Action by |
Due Date |
Status / Comments |
Date closed |
|---|---|---|---|---|---|---|---|
Report | of medical administrative support. Recognising the higher turnover of admin colleagues, a job description review is underway, with the Education and Development team leading a review of admin career development. The employee experience team will be prioritising admin colleagues for the Talent Management Plan. Propose to close this action on the Board log and monitor progress with the action at People and Culture Committee. | ||||||
23.48b | 28/09/23 | People and Remuneration Committee Chair’s Report | To update on the framework used for exit interviews. | Cath Byford | November 2023 | Exit Interview process will be taken to People and Culture Committee following 12 months since the implementation of the new online methodology. Exit interview dashboard now in testing phase with demos shown to the Culture Pillar | 23/11/23 |
|
Agenda item number |
Date |
Item |
Action |
Action by |
Due Date |
Status / Comments |
Date closed |
|---|---|---|---|---|---|---|---|
with ‘go live’ from January 24. Propose to close this action on the Board log and monitor progress with the action at People and Culture Committee. | |||||||
23.50g | 28/09/23 | Operational Performance | To check on progress with the recording of physical health checks on Lorenzo | Jason Hollidge | November 2023 | Due to unforeseen staff absence unable to obtain the data to provide the update this month | |
23.50h | 28/09/23 | Operational Performance | To formally thank the Talking Therapy team for their improved performance. | Jason Hollidge | November 2023 | Team thanked. More comms planned to showcase improvements | 23/11/23 |
23.51a | 28/09/23 | Strategy | To allow more time on the agenda for discussions on strategy, finance and operational performance. | Jean Clark | November 2023 | November agenda reflect request. | 11/10/23 |
|
Report to: |
Board of Directors |
|---|---|
Meeting date: | 23rd November 2023 |
Title of report: | Chair’s Report |
Purpose of paper: | For Information and assurance |
Author: | Zoë Billingham, Chair |
Link to Trust Strategy | All strategic objectives of new Trust Strategy: Inspirational people, exceptional care, transforming lives |
Legislation/Compliance | CQC Well-led |
Link to BAF Risk/s | Links to all the risks on the Board Assurance Framework, in line with our Trust Strategy – key BAF risks included in appendix |
Executive summary
This is a summary report from the Chair covering the last two months.
Recommendation
The Board is asked to note this report.
Chair’s Report
-
Appointment of our new Chief Executive Officer - Caroline Donovan
-
Since our last meeting, we have had a change of leadership within NSFT, following Stuart Richardson’s departure at the end of October. I would like to place on record, my personal thanks to Stuart for his enormous contribution to supporting the Trust and our service users and staff through some very challenging times.
-
I was delighted to welcome Caroline Donovan as our new CEO when she formally took up her post on 1 November. Caroline is an experienced mental health chief executive, with an excellent leadership track record, and brings with her a wealth of knowledge and experience that will be invaluable to us as we continue our journey of improvement. I am confident she will bring renewed focus and impetus to ensuring NSFT provides high quality, person-centred and compassionate care, while being a great place to work for our staff.
-
Annual General Meeting and Annual Members Meeting
-
It was wonderful to be able to hold this year’s Annual General Meeting and Annual Members Meeting in person once again this year, after two years of having to meet remotely. Over 100 people joined us on 7 November at The Mix in Stowmarket, where 11 of our Trust teams and partners took part in a marketplace event, held immediately before our formal meeting. Staf, partners and service users and carers were able to showcase a wide range of the improvement projects under way across our two counties. People with lived experience of mental health illness explained their vital contributions and made this event a truly inspirational experience for all of us in there.
-
The stall showcased the Trust is undertaking including an update on the multi-million- pound Rivers Centre development at Hellesdon, Particip8 – a group that gives young people a voice in making improvements to the services they use, and the Healthwatch Serious Mental Illness (SMI) project – a collaborative which aims to ensure carers of those with serious mental illness are supported in their vital roles.
-
In the formal meeting that followed, the Trust Board members shared their reflections on the past year, and also outlined the Trust’s Strategy for the future, which has been shaped with full involvement of staff and people who use the Trust’s services.
-
Wedgewood Therapy Garden – a collaborative venture to support service users and our community
-
Last month I had the absolute pleasure of attending an inaugural event to celebrate the Green Minds Wedgwood Therapy Garden on the west Suffolk Hospital site in Bury St Edmunds. This was such an inspiring and uplifting event, where I joined representatives from the local voluntary sector, Trust staff and patients and project members to see the wonderful new garden and hear about exciting plans for its future. Following two years of tireless fundraising the project has truly transformed what was once a green wasteland into a biodiverse, sensory garden for use by patients, staff, carers, and vulnerable members of the wider community to promote the benefits of outside spaces in supporting good mental health.
-
This project has demonstrated so perfectly just what can be achieved through collaboration with our local charities and community groups. This garden will offer vulnerable people in the wider community year-round gardening workshops. It offers a place of recovery and reflection as well as a hub for therapeutic horticultural activities. Creative workshops including art, crafts and seasonal sessions will also be included.
-
Medical Staffing Committee and Board joint meeting
-
Last month I chaired our joint Medical Staffing Committee and Board meeting, which provides an important opportunity to discuss how we ensure that our medical leaders are at the heart of the Trust’s management and improvement agenda. It was a thought provoking facilitated session where we identified actions that will lead to tangible improvements in medical staff engagement and support. A clear programme of priorities has been identified through the Group’s productive debate and discussion. It was encouraging to see some quick wins starting to emerge around mentoring, defining of roles and the absolute necessity for Executive visibility with medical colleagues. Whilst this group is relatively new, it is starting to demonstrate significant value in supporting our improvement journey.
-
System working, engagement and our services in action
-
One of my key priorities as Chair is to ensure that the Trust plays a full and active part in engaging with our system partners, the voluntary sector and our service users and carers in improving integrated mental health provision across Norfolk and Suffolk. Having visited
-
the hospital over the summer I was pleased to invite Tom Spink the Chair of the Norfolk and Norwich University Hospital to accompany me on a visit to a number of our Hellesdon wards. We discussed ways in which we can work better together in order to support service users and patients requiring mental and physical health support. Tom was delighted to meet many of our staff and service users and was truly impressed with the care that we provide. He told me ‘I thought every member of staff I met was superb and all demonstrated that wonderful ability to engage with your patients in such a caring manner’.
-
In late September I had the pleasure of joining the Suffolk Parent Carer Forum at their Open Forum event in Ipswich. It brought together a wide range of voluntary organisations whose aim is to support families in navigating the complexity of healthcare provision in Suffolk and to advocate for change and improvement.
-
If we are to tackle mental health inequalities effectively across our two counties there must be effective system working and to that end, I have participated in a range of events designed to improve joint working. Through my membership of the ICB Chairs’ network I am able to build relationships with my peers from across the ICB family. The Norfolk & Waveney ICB has been working together to continue in strengthening system links. To this end a facilitated workshop for Chairs was held and provided a great opportunity for us to look further at collaborating on priorities and development needs across the system. We we are identifying changes we can make though joint working that improve the lives of the populations we serve.
-
Earlier this month I participated in the launch of an important new ICS System Learning programme for the Suffolk and North East Essex Integrated Care System. ‘Uncomfortable Truths’ which brought together leaders from across the ICS to work jointly on the very important issue of how we can improve culture in our local health and care
system. Whilst we have lots of plans and strategies in place to deliver the best health and care services for our population, we know that if we are to genuinely ‘Turn the Curve’ on the outcomes and experiences for local people, communities, and our staff we need to look deeper, and consider the underlying culture of our health care system. This event focused on exploring ‘Uncomfortable Truths’ about our health and care system including safety, inclusivity and improvement.
-
This month I attended the ‘Falling Through the Cracks’ conference hosted by Restitute, a Community Interest Company focused on supporting victims of crime. The day was very interactive with scenario-based discussions on the important topic of sexual abuse and the terrible impact this can have on survivors’ and their families’ health, well-being, and mental health. I valued being included in a panel discussion looking at how we can make sure all family members are supported and that people are not forgotten, both at the point of disclosure and in the years that follow. I came away with such a sense of renewed optimism that together with our partners we are not just talking about making improvements, we are now tackling important issues and identifying joint action that will change outcomes for people in our communities.
-
Non-Executive Directors (NEDs) visits
-
The NEDs have visited two services since the last Board meeting:
-
Lindsey Hoy visited Chatterton House in Kings Lynn where she and the Trust’s Freedom to Speak Up Guardian met with the Deputy Director of Service and a number of staff members. They also joined a ward round and met staff from the CRHT, Community and Admin teams. The visit was undertaken jointly with the Trust’s independent Freedom to Speak Up (FTSU) Guardian as a direct response to an increasing number of FTSU cases raised from the site over recent months. The Deputy Services Director welcomed the increase in leadership visibility and the welcomed the opportunity to discuss the issues being raised and activity to help improve. During the site visit both the Freedom to Speak Up Guardian and Ms Hoy met individually with staff members to understand and discuss concerns.
-
Tricia Fuller visited the Home Treatment Team at Wedgewood House in Suffolk, where she met with the team and heard about the pressures on the service, which has high and unpredictable demand and faces staffing capacity challenges. Tricia was very impressed with the leadership and the professionalism of the team. Regardless of the capacity challenges, the culture within the team was excellent, with positive feedback from both clinical and administrative team members.
-
-
Council of Governors
-
It has been a busy time for the Council of Governors who met twice in October. At last month’s Council of Governors meeting an update about the work around strengthening clinical and operational leadership was discussed along with updates on various engagement sessions that had taken place.
-
The Council of Governors met on 9 October and sought assurance and progress on the learning from deaths work. Governors also requested an update on ‘right care right person’, an operational model developed by Humberside Police that aims to change the way the emergency services respond to calls involving concerns about mental health. A full update will be provided to the next Council of Governor meeting in public on 14 December.
-
I was also delighted to chair a joint meeting of the Council of Governors and the Board of Directors on 26 October where we reviewed progress on the Trust the strategy, including future focus. The governor priorities, developed from member feedback, were also reviewed and discussions focused on what additional assurance was required. Governors were also able to meet Caroline Donovan, who attended the meeting in a shadowing capacity during her hand over period.
-
Four prospective governor events were held during October to attract new governors to apply for the available positions. Two events were online and two were in
person. Nominations are now closed, and voting will take place between Friday 17 November and Friday 8 December 2023 with results announced at the Council of Governor meeting held in public on Thursday 14 December 2023. There was one uncontested seat, and we will be welcoming Sheila Preston as a Suffolk public Governor from 1 February 2024.
|
Report to: |
Board of Directors |
|---|---|
Meeting date: | 23rd November 2023 |
Title of report: | Chief Executive Officer’s Report |
Purpose of paper: | For Information and assurance |
Author: | Caroline Donovan, Chief Executive Officer |
Link to Trust Strategy | All strategic objectives of new Trust Strategy: Inspirational people, exceptional care, transforming lives |
Legislation/Compliance | CQC Well-led |
Link to BAF Risk/s | Links to all the risks on the Board Assurance Framework, in line with our Trust Strategy – key BAF risks included in appendix |
Executive summary
This is a summary report outlining my first few weeks as Chief Executive.
Recommendation
The Board is asked to note this report.
Chief Executive Officer’s Report
-
Introduction
-
I am delighted to have taken up this position at the beginning of the month. I am grateful to former CEO, Stuart Richardson, for spending time with me prior to this to facilitate a smooth handover. I know that the Trust has already paid tribute to Stuart for his leadership up to this point and the impact he has had which is borne out in the improvements that are already under way.
-
My background as a nurse has given me focus throughout my career on the delivery of high-quality patient care. I am passionate about mental health services and the people who require them, their families and carers and of course, the staff who provide them.
-
Prior to joining NSFT, I was the Chief Executive of Lancashire and South Cumbria NHS Foundation Trust, a mental health and learning disability provider of a similar size and geographical spread. I was also Chief Executive at North Staffordshire Combined Healthcare NHS Trust, a provider of mental health, social care, learning disability and substance misuse services which was rated ‘Outstanding’ by the CQC under my leadership.
-
My initial focus has been on meeting our staff, key partners and stakeholders and making sure I am fully sighted on the Trust’s challenges and continuing improvement journey.
-
Initial Priorities
-
I am fully focused on the Trust’s continued improvement journey together with staff, service users and carers and with partners and our communities. My emerging priorities are four-fold and very much aligned to the thoughts and ideas that many people have had as part of the formation of the Trust strategy:
-
Improving Health – working with partners to improve outcomes for service users and carers, and tackle inequalities
-
Improving Quality – developing our Quality Strategy and ensuring safe, effective, personalised care; and service users are able to access our services in a timely manner
-
Improving our Culture and Staff Experience – Ensuring our staff feel supported and safe to speak up, and that they have the resources and environment to flourish
-
Improving Value – making sure we deliver value in all that we do, in how we make effective use of resources and transform our pathways of care, with partners, to improve performance.
-
-
In addition, I am committed to openness, honesty and transparency in all our communications and relationships.
-
Engaging with our Staff and Stakeholders
-
I was particularly pleased to take part in the ‘Hear to Listen’ on my first day, which gave me the opportunity to speak directly to the 350+ staff who joined in and discuss my priorities with them.
-
I have participated in two workshops with our Trust Board and our Council of Governors both of which were focussed on our continuing improvement. We all have a common purpose and ambition to get the Trust to where it needs to, and indeed can, be.
-
I have begun a series of visits to services which will, wherever possible, include a ‘drop in’ element to enable to any members of staff to come and meet me. The first of these was on 9th November when I visited our wards in Hellesden Hospital. I was able to talk to a range of staff there including ward staff and members of the crisis team and listen to their progress, concerns, and ideas. I am very much looking forward to more such meetings and visits going forward.
-
On 14th November I hosted the first of our new style Senior Leadership Team meeting which included network leads as well as executives. I reinforced the need for all leaders to focus on staff and ensuring their role modelling of behaviours and values filters down throughout the organisation to engender authentic openness and transparency.
I have been impressed with the staff I have met so far, particularly by their ‘can-do’ attitude and obvious commitment to service users and carers. It is vital that this is supported and facilitated by leadership.
-
I have been formally appointed to both the Norfolk and Suffolk Integrated Care Boards and attended their meetings later in the month. This is fundamental to our commitment to work in partnership and collaborate with health and social care organisations (as well as others) in our patch.
-
On 15th November, Chair Zoe Billingham and I met with our MPs in Westminster which gave us a great opportunity to set out our plans for continuing improvement as well as listen to their feedback, views and any concerns.
-
My personal, fortnightly blog is published on Mondays (there have been two to date- 6th and 20th November) and this is widely distributed to all stakeholders. If you are not on the mailing list for this publication and would like to be included, please let us know.
-
Annual General Meeting and Annual Members Meeting – held on 7 November.
-
Our Annual General Meeting and Annual Members Meeting, held at The Mix in Stowmarket, was a great success. It gave multiple Trust teams the chance to showcase their improvement projects in a market stall area. There is more detail on this in the Chair’s Report. was delighted to be able to share my early thoughts and priorities with the audience and to take part in a panel question and answer session, which was both insightful and positive.
-
Showcasing NSFT’s specialist services to England’s Chief Nurse
-
On 6 October, Dame Ruth May, England’s Chief Nursing Officer visited NSFT to find out more about the ground-breaking services it offers to veterans and the innovative support it provides to its staff across Norfolk and Suffolk.
-
She heard about the Veterans’ Integrated Services and Operation Courage, which brings a range of mental health, financial and housing support into one place to make it easier to access. Staff also explained more about the support which is available to colleagues. This includes the Trauma Risk Incident Management (TRIM) Service, which sees peers offers help to people impacted by difficult incidents at work, and services which support BME staff and international nurses.
-
Award successes
-
NSFT and partners win coveted healthcare innovation award
-
A collaboration between Norfolk and Suffolk NHS Foundation Trust (NSFT) researchers, Eastern Academic Health Science Network (EAHSN) and BFB Labs, was named the winner of the outstanding contribution to population health through innovation award at the second annual Innovate Awards. The award-winning project focused on tackling a critical issue in child mental health – anxiety disorders among children aged 7-12 years. With at least 500,000 children in the UK falling within this age group estimated to be experiencing anxiety difficulties, it represents a significant concern for the NHS.
-
Recognising the urgent need to address this challenge in mental health care, NSFT researchers with their partners set out to evaluate 'Lumi Nova: Tales of Courage', a digital therapeutic game to learn more about using digital therapeutic tools in young people’s mental health services. Lumi Nova, developed by BFB labs, delivers NICE-recommended therapy via an immersive app-based game which helps to alleviate anxiety symptoms in young people.
-
The findings suggest that digital interventions are a good treatment option for some children with anxiety, which will enable more young people to access the mental health support they need, when they need it.
-
-
NSFT nurse wins prestigious UK award for improving dementia diagnosis and care.
-
Kumar Ponnusamy nurse consultant at NSFT was announced the winner in the Nursing Older People category of the RCN Nursing Awards 2023 at a ceremony on Friday 10 November at Liverpool Cathedral.
-
Mr Ponnusamy created a memory assessment service to improve dementia diagnosis and treatment in care homes to address the NSFT memory clinic waiting list. After producing a business case and designing a clinical pathway for the service, he created nurse-led multidisciplinary meetings for case discussion, diagnosis and devising care plans, including reviews of antipsychotic medication.
-
The award recognised not only the hard work of those involved, but the benefit of NSFT being people-led as part of the Trust’s Improvement Programme. By valuing the work of our award-winning and inspirational staff the Trust continues to improve our care and deliver high quality services for patients.
-
-
NSFT nurse features in national recognition of exceptional women for Black History Month
-
The theme for this year’s Black History Month was ‘Saluting our sisters, celebrating the exceptional achievements of black women’.
-
Priscilla Nzounhenda, the Trust’s Deputy Lead Nurse for Secure Services and co-chair of the BME Staff Network, was one of four black women across NHS Providers’ national membership invited to give her reflections on her challenges and achievements in her NHS career and set out her message to NHS leaders on their role in tackling racism.
-
Priscilla’s contribution can be read here: Saluting our sisters: celebrating the exceptional achievements of black women (nhsproviders.org).
-
The trust also celebrated Black History Month at a special event held at The Willow Centre, Cringleford, Norwich on 23 October. Attendees celebrated achievements over the last year and discussed the barriers that still need to be broken down. Tendai Ndongwe, Deputy Head of Equality Diversity and Inclusion from NHS East of England delivered the keynote of the day, focusing on the importance of Black History Month, anti- racism, and of course, saluting our sisters.
-
-
Annual Staff Awards
-
On Thursday 16th November, we celebrated the Annual Staff Awards at a glittering ceremony in Trinity Park, Ipswich. More than 200 members of staff and service users gathered to recognise the fantastic work by a multitude of people, which is having a direct impact on our improvement journey.
-
This has been a record year for the Awards with more than 460 nominations for individuals and teams across nine categories. There was also a Special Recognition Award.
-
Judging panels consisted of executives, non-executive directors and people with lived experience, and they had the near impossible task of choosing winners from the, without exception, excellent entries.
-
At the time of writing, winners have not been announced and I very much look forward to updating you further at the Board meeting.
Date: 23rd November 2023 Item: 23.57
Strategic Objective 3 – Transforming Lives
Risk Description 3.1 Risk of failure to gain and sustain the confidence of the service users, partners, other stakeholders and public
Risk Appetite – the Trust has an open risk appetite in gaining the trust and confidence of our service users, partners and wider public
Date last reviewed:
November 2023
Director Lead:
Caroline Donovan CEO
Board Committee:
Board
Consequence of risk:
If the Trust fails to gain the confidence of stakeholders this impacts on ability to transform and improve services in partnership, on CQC rating and RSP and financial sustainability
Target Rating: (l x c) and Date to reach target
3 x 4 Q3 2024/25
Risk Rating over time
25
20
15
10
5
0
Rationale for current score: (l x c) Collaborative working to improve learning from deaths and addressing remaining CQC must dos.
Controls (what are we currently doing about the risk?)
-
Trust Improvement Programme. N&W chairing Evidence Assurance Group (EAG) which signs of CQC must dos and
Jan-23 Mar-23 May-23 Jul-23 Sep-23 Nov-23
Assurances (how do we know if the things we are doing are having impact?)
-
Improvements highlighted by CQC report published February 2023. Overall rating improved to ‘Requires Improvement’. No enforcement notices.
Improvement Board with system partners and key stakeholders
-
New CEO is member of both Integrated Care Board (ICB) boards
-
NSFT is active partner of Norfolk & Waveney and Suffolk & North East Essex ICBs MH collaboratives and EoE Provider Collaborative
-
Working with regional and national MH Trusts. Regional and system colleagues attend Quality Assurance Committee, Performance & Finance Committee and participate in Quality & Safety Reviews
-
Experience of Care Committee with partners, service users, Healthwatch
-
Progress with Improvement programme phase 2 with partners, and continued progress with CQC must dos and Improvement Board monitors metrics. But Trust remains in Recovery Support Programme (RSP)
-
Positive progress with east of England provider collaborative performance metrics.
-
Progress with recommendations from the Grant Thornton UK LLP’s audit of the processes the Trust uses to collect and report mortality data. Learning from deaths report to the November Board.
-
Progress on actions reviewed at each Joint Board MSC meeting
|
Date: |
23rd November 2023 |
Dii |
|---|---|---|
| Item: | 23.57 |
|
|
|---|---|
Gaps
| Mitigating actions (what more should we do?)
|
|
Report to: |
Board of Directors |
|---|---|
Meeting date: | 23rd November 2023 |
Title of report: | Freedom To Speak Up Report |
Purpose of paper: | For information and assurance |
Author: | Ade Adetukasi, Associate Director of Employee Experience & OD Kym Gillingham, Freedom To Speak Up Guardian |
Director: | Cath Byford, Deputy Chief Executive/Chief People Officer |
How this paper impacts on Trust Strategic Objectives | Engage, develop, inspire our staff. The paper is linked to the Improvement Plan Culture Pillar. |
Legislation/Compliance | Public Interest Disclosure Act 2010 Freedom to Speak Up national guidance |
How this paper impacts on current risks in Corporate Risk Register or BAF | Board Assurance Framework (BAF) risk 1.1 |
-
Executive summary
This paper provides the Board with an update on the activities of the Freedom to Speak Up (FTSU) service as provided by the Guardian Service Limited (GSL). The paper provides a summary of key highlights from the September FTSU report and other notable activities.
There is emerging evidence that the growing confidence in the FTSU service is beginning to encourage a speak up culture in the Trust. Though the September report shows a drop in the number of cases raised, we are noticing a boarder use of the FTSU service by both staff and managers. For the first time since the service was launched in November 2022, the guardian was twice approached by staff in September to support resolution of local issues. This was achieved without the need for escalation to senior management or for formal processes, with the staff members feeling supported.
Based on the reported “outcomes after action taken” in the September report, the FTSU service is not only enabling staff to speak up, learning from concerns resolved are leading to positive change and improving outcomes. Below are examples of some of the recently reported outcomes following actions taken in response to issues escalated by the FTSU guardian:
-
Reviews been conducted into quicker access to beds with an appropriate home support put in place in the interim.
-
Service Director acknowledged long waits for assessments and has escalated the issue for further action.
-
Staff member has returned to work following a period of sickness absence.
We recognise we need to get better at listening up including how we support staff who speak up, and how we enable a safe environment for staff to speak up without the fear of detriment.
According to recent research by Professor Reitz and John Higgins on speak up culture, “Whilst bravery and speak up skills have a role – the focus is a complete waste of time and resources unless those in position of power are able and willing to make it safe for others to speak up – and listen up in a way that makes them want to speak up again.”
-
Key highlights from the September 2023 FTSU data.
-
There is a noticeable drop in the number of new cases raised and for the second month in a row as shown in Appendix 1 below. Compared to 35 new cases raised in July, there were 18 new cases raised in September. This is particularly significant as there is a corresponding increase in the wider use of the FTSU service as an independent support resource by both staff and managers who are speaking up with a desire for resolution of issues without the need for instigating escalation or formal procedures.
-
In terms of themes, the majority of the new cases reported in September were regarding “Systems & Processes” and “Patient Safety”. All the patient safety related cases were escalated to lead nurses or the patient safety team, and all were promptly responded to and staff members who raised these concerns duly supported by the guardian.
-
A review of the systems and processes related cases showed there were mostly concerns about lack of clarity or poor application of policies or processes. The reported cases included:
-
Concerns about recruitment process not been followed in some services and teams.
-
Concern about the process of referring service users to other services.
-
Concern about the transfer policy on handover of services users from one team to another.
-
Concern about the introduction of changes to local team structure without consultation.
The guardian continues to work closely with local managers to resolve and respond to staff who raised these concerns.
-
The growing staff confidence in the FTSU service is beginning to enable a broader use of the service. As mentioned above, and for the first time since the service was launched in November 2022, the guardian was twice approached by staff in September to support resolution of local issues within the context of a facilitated meeting. Facilitated meetings are informal meetings specifically arranged to resolve concerns without the need for escalation or a formal process and within the scope of the FTSU service. Where appropriate, the guardian is only present for support and to provide a
safe space for staff and managers to discuss issues with the goal of achieving resolution.
-
To encourage people to speak up and use the service, as part of the October 2023 Speak Up month, the photograph of the FTSU guardian and details of the service were displayed on the front page of the intranet and used as screen savers throughout October. In addition, we published series of news article on the service on the intranet, the weekly Trust Update, and in the weekly managers briefing emails. Below are some of the recent feedback from staff who have used the service.
‘Thanks again, just wanted to say that staff members of our team feel very supported by yourselves after the presentation in MDT recently!’’
‘Thanks for your help and for being so responsive to my concerns. I felt your presence at our meeting today was positive and have since spoken to a couple of members of staff who may be raising matters with you.’
‘Sadly, I have had to use the ‘Speak up service’ on 2 occasions recently. However, what has made this easier is Kym’s reassurances, her ability to listen without judgement and ask appropriate questions to the situation. In both incidents Kym has been very proactive, not only in her very quick response/meeting with me but also letting me know who she will be escalating the concerns to and providing me with feedback once this has been completed.”
-
Next steps
-
We have commenced the process of putting in place a medium-term plan for a highly functioning FTSU services. In recognition of the need for an independent FTSU service, and to strengthen NSFT’s speak up culture, the Trust outsourced the FTSU service to GSL on an initial 12 month contract due to expire on 14th November. The executive team have approved the recommended 12 months extension to the current contract with GSL (with the option of a further additional 12 months extension), based on an options appraisal.
-
As part of the Trust’s response to the Lucy Letby case, especially in relation to supporting staff who may be experiencing cultural barriers to speaking up, we are co-developing a survey for staff in protected characteristics groups. The goal of the survey is to gather information and understand existing or potential cultural barriers stopping staff from minority groups from speaking up. This is particularly important as the current format of the monthly FTSU data produced by GSL does not include demographic data to ensure confidentiality. We plan to launch the survey in January 2024.
In addition, we are in the process of bringing together a multi-disciplinary task and finish group (including the patient safety and customer service teams among others) to develop and implement a central log for all concerns and consider resource requirements for ensuring a robust response to FTSU cases. The scope and timeline for the task and finish group will be reported at the next People and Culture Committee meeting in January 2024.
-
Following a review of the Trust’s FTSU policy, the Policy Working Group has approved the adoption of the new NHS England FTSU policy as the new local NSFT FTSU policy in line with national guidance. The new policy was ratified at the November Trust Partnership Meeting (TPM). The new guidelines set out a simple process and national standard on what should happen when staff speak up.
-
Quality implications
-
a. The paper outlines additional measures to strengthen the FTSU service and this will improve quality.
-
Impact on people who use services and their carers
a. The strengthened FTSU safeguards will provide assurance to service users and carers.
-
Equality implications
a. FTSU cases are reviewed by theme to understand implications for protected characteristic, any discrimination and inequality and to ensure no staff member suffers a detriment because of speaking up. The strengthened processes better support that.
-
Financial implications
a. There are additional financial implications for strengthening processes to support FTSU and patient safety and these will be set out in a separate paper.
-
Risks and mitigations
a. The key risk with FTSU is staff feeling concerned they will suffer detriment in speaking up. The new independent guardian, swift response and wider communications is encouraging more staff to speak up and enabling an open culture.
Appendix 1
Appendix 2



 Appendix 4
Appendix 4
 Appendix 6
Appendix 6

|
23 |
26 |
|---|---|
|
0 |
Appendix 8

|
Report To: |
Board of Directors |
|---|---|
Meeting Date: | 23rd November 2023 |
Title of Report: | Audit & Risk Committee Chairs’ Reports |
Purpose of report: | For assurance and approval |
Authors: | Lindsey Hoy, Non-Executive Director |
Director: | Zoe Billingham, Chairperson |
Link to Trust Strategy | Links to all Strategic objectives |
Legislation / compliance | CQC Well-Led; NHSE performance framework |
Link to BAF / Risks | All risks on Board Assurance Framework as each Committee reviews those relevant to its terms of reference |
Executive Summary:
This report provides information, assurance and escalations from the meeting of the Audit and Risk Committee held on 8th November 2023.
Recommendation
The Board is asked to note the report
Chairs Report – Audit and Risk Committee Meeting 8th November 2023 Positive Assurances
A positive verbal update on initial External Audit planning was received.
The Internal Audit Team demonstrated good progress against the 2023/24 Internal Plan which remains on track, and the audit report for Financial Management was presented which received an overall 'Reasonable Assurance' rating. Highlights of initial discussions with the Executive teams on the 2024/25 plan were shared along with a proposal to include a Safeguarding audit instead of a Lorenzo audit on the next years plan. (As this is not a current year audit change, it did not require Committee approval).
The Clinical Audit Programme continues to evolve. Audits per the agreed plan are being conducted with good levels of completion from the teams involved. However, activity to reduce the volume of open actions from clinical audits has not yet had the outcome expected. A revised plan has been implemented to review open actions, cleanse the data and coach staff who are using the MEG audit tool. A reduction in the approximately 900 open actions is expected in the next reporting period.
The Counter Fraud Team reported good progress against the 2023/24 counter fraud annual plan, with activity progressing to plan.
NSFT Improvement Programme update identified workstreams continue to remain largely on track. Overarching controls which reduce the Programme Risks were discussed, including how assurance is gained that key controls or mitigations the Programme team rely on to reduce programme risks are operating effectively. A short paper will be presented at the next Committee on this topic. Outcomes reporting, which include key metrics to demonstrate improvements being made in the Programme are having the desired impact, have been piloted and in January 2024 will
be shared with each relevant Board Sub-Committee along with their usual workstream updates to demonstrate the impacts from programme work.
Compliance reports identified no significant adverse Single Tender Waiver trends, Information Governance events or employment Tribunal settlements outside the norm. A paper on Consultancy cost controls was received which the Committee welcomed. This has highlighted where enhancements should be made to controls, some of which have already since been implemented. The final report and findings are still being collated (see 'matters of concern' below) and the final outcomes and action plan will be bought back to the next Committee.
Risk Management reporting noted Risk Training will now become a mandatory module for relevant staff across the NSFT which was welcomed.
Actions which were escalated from the last Committee were discussed and next steps noted. TAC Cards and also Your Data / Your Choice issues will be subject to re-review early in 2024 to identify if recent actions have had impact. An update on Counter Fraud Section 12 work was given as part of updating open cases in the committee meeting, with further updates due in January 2024.
Actions to identify loggists was reported as progressing, and an update will be given in March 2024 in the 6 monthly Emergency Preparedness Resilience Response (EPRR) update.
Decisions Made
Changes to the target date for 3 open audit recommendations were not approved as these did not meet the criteria for changing target dates. The Committee reminded those who create plans to address audit recommendations to ensure plans are robust, timescales are achievable, and activity remains at pace to meet timescales agreed.
The Terms of Reference were agreed for recommendation to the Board.
Matters of concern and key risks to escalate
The volume of overdue audit recommendations is of concern to the Committee. This is currently running at 24% of audit recommendations are overdue and Board members are urged to review open recommendations and take appropriate actions to close.
The volume of risks on the corporate risk register not updated is increasing, which is disappointing after improvements were seen when the Committee used a 'Comply or Explain' approach in early 2023. Updating open risks with progress is a key part of risk management and can be one barometer of how embedded risk management is across the Trust. The Board are urged to review the Trust governance and processes for risk management and embed process across all areas and all levels of the Trust.
Responses to Committee Effectiveness questionnaires have been very low in other Board Sub Committees. ARC request all members of Board Committees please respond to the Questionnaires so that Boards Effectiveness can be assessed.
A recent internal review into Consultancy cost controls is near completion, with final responses to questions needed from the Senior Leadership Team. This will allow full results and enhancements to the control framework be presented at the next ARC.
Major actions commissioned / work underway
Clinical Audit Team to enhance reporting on open actions to give a size of impact to the Trust.
Reporting to the Audit and Risk Committee of Fraud Cases that are being followed up with HR will be enhanced to allow the Committee adequate oversight of outcomes.
AUDIT AND RISK COMMITTEE TERMS OF REFERENCE
-
CONSTITUTION
-
The Trust Board hereby resolves to confirm the constitution of a Committee of the Trust Board to be known as the Audit and Risk Committee (The Committee), which is directly accountable to the Trust Board.
-
The Committee is a non‐executive committee of the Trust Board and has no executive powers, other than those specifically delegated in these terms of reference.
-
All procedural matters in respect of conduct of meetings shall follow the Trust’s Standing Orders.
-
-
PURPOSE
-
The Committee is responsible for the establishment and maintenance of an effective system of integrated governance, risk management and internal control, across the whole of the Trust's activities (both clinical and non- clinical), that supports the achievement of the Trust's objectives.
-
-
MEMBERSHIP
-
The Committee shall be appointed by the Board from amongst the Non‐Executive Directors of the Board and shall consist of not less than three Non‐Executive Directors. The membership shall include representation from other Board Committees.
-
The Chair of the Trust shall not be a member of the Committee.
-
A quorum shall be two members.
-
The Chair of the Committee shall be appointed by the Board.
-
All members are expected to attend each meeting.
-
The Chief Finance Officer, the Head of Internal Audit, The Local Counter Fraud Specialist and a representative of the external auditors shall normally attend meetings. The Committee has the right to meet with the internal or external auditors without Executive Board members being present.
-
The Chief Executive and other Executive Directors should be invited to attend, but particularly when the Committee is discussing areas of risk or operation that are the responsibility of that Director.
-
The Chief Executive should be invited to attend, at least annually, to discuss with the Audit and Risk Committee the process for assurance that supports the Annual Governance Statement.
-
-
FREQUENCY OF MEETINGS
-
Meetings shall be held not less than four times a year. The External Auditors or the Head of Internal Audit, Chair or any other Non‐Executive Director may request a meeting if they consider that one is necessary.
-
-
AUTHORITY
-
The Committee is authorised by the Board to investigate any activity within its terms of reference. It is authorised to seek any information it requires from any employee and all employees are directed to co‐operate with any requests made by the Committee.
-
The Committee is authorised by the Board to obtain outside legal or other independent professional advice and to secure the attendance of outsiders with relevant experience and expertise if it considers this necessary.
-
-
DUTIES AND RESPONSIBILITIES
-
The duties of the Committee can be categorised as follows:
-
Governance, Risk Management and Internal Control
-
Whilst recognising the Committee has an overriding and absolute responsibility for reviewing financial controls, the Committee shall also review the establishment and maintenance of an effective system of integrated governance, risk management and internal control, across the whole of the organisation’s activities (both clinical and non‐ clinical), that supports the achievement of the organisation’s objectives.
-
The Board of Directors has the responsibility of setting the risk appetite for the organisation. The Audit and Risk Committee will periodically review the implementation of the risk appetite as part of risk management and internal control.
-
In particular, the Audit and Risk Committee will review the adequacy of:
-
All risk and control related disclosure statements (in particular the Annual Governance Statement), together with any accompanying Head of Internal Audit statement, External Audit opinion or other appropriate independent assurances, prior to endorsement by the Board
-
The underlying assurance processes that indicate the degree of the achievement of corporate objectives, the effectiveness of the management of principal risks and the appropriateness of the above disclosure statements
-
The policies for ensuring compliance with relevant regulatory, legal and code of conduct requirements
-
The policies and procedures for all work related to fraud and corruption as set out in Secretary of State’s Directions and as required by NHS Counter Fraud Authority
-
Arrangements by which staff may raise, in confidence, concerns about possible improprieties in matters of financial reporting and control, clinical quality, patient safety or other matters (Whistleblowing Policy and Procedure). The Committee should ensure that arrangements are in place for the proportionate and independent investigation of such matters and for appropriate follow‐up action.
-
-
In carrying out this work the Committee will primarily utilise the work of Internal Audit, External Audit, regulators and other assurance functions, but will not be limited to these audit functions. It will also seek reports and assurances from directors and managers as appropriate, concentrating on the over‐arching systems of integrated governance, risk management and internal control, together with indicators of their effectiveness.
-
This will be evidenced by the receipt of Internal Audit reviews of Risk Management, Control & Review Processes to support the Annual Governance Statement, and consideration of the Board Assurance Framework when approving the Internal Audit programme.
Internal Audit
-
The Committee shall ensure that there is an effective Internal Audit function established by management that meets Mandatory Public Sector Internal Audit Standards and provides appropriate independent assurance to the Audit and Risk Committee, Chief Executive and Board. This will be achieved by:
-
Consideration of the provision of the Internal Audit service, the cost of the audit and any questions of resignation and dismissal.
-
Review and approval of the Internal Audit strategy, operational plan and more detailed programme of work, ensuring that this is consistent with the audit needs of the organisation as identified in the Board Assurance Framework
-
Consideration of the major findings of Internal Audit work (and management’s response) and ensure co‐ordination between the Internal and External Auditors to optimise audit resources
-
Ensuring that the Internal Audit function is adequately resourced and has appropriate standing within the organisation.
-
Monitoring the implementation of recommendations resulting from Internal Audit reports.
-
Annual review of the effectiveness of Internal Audit.
-
External Audit
-
The Committee shall ensure compliance with the National Health Service Act 2006 and the Audit Code for NHS Foundation Trusts in relation to the appointment and provision of an external audit service.
-
The Committee should make recommendations to the Council of Governors in relation to the appointment, re‐appointment and removal of the External Auditor and approve the remuneration and terms of engagement of the External Auditor.
-
The Committee shall review the work and findings of the External Auditor appointed by the Council of Governors and consider the implications and management’s response to their work. This will be achieved by:
-
Assessing the External Auditor’s work and fees on an annual basis to ensure that the work is of a sufficiently high standard and that the fees are reasonable, including the use of performance measures, as appropriate.
-
Reviewing and monitoring the External Auditor’s independence and objectivity and the effectiveness of the audit process, taking into consideration relevant UK professional and regulatory requirements.
-
Making recommendations to the Council of Governors with respect to the re‐ appointment of the External Auditor, following the annual assessment.
-
Discussion and agreement with the External Auditor, before the audit commences, of the nature and scope of the audit as set out in the Annual Plan, and ensure co‐ordination,
-
as appropriate, with other External Auditors in the local health economy.
-
Discussion with the External Auditors of their local evaluation of audit risks and assessment of the Trust and associated impact of the audit fee
-
Review all External Audit reports, including agreement of the annual audit letter before submission to the Board and any work carried outside the annual audit plan, value for money reports and management letters, together with the appropriateness of management responses.
-
Monitoring the implementation of recommendations resulting from external audit reports.
-
If required, develop and implement a policy on the engagement of the external auditor to supply non‐audit services, taking into account relevant ethical guidance regarding the provision of non‐audit services by the external audit firm.
Local Counter Fraud Specialists
-
The Committee shall ensure that there is an effective and appropriate Local Counter Fraud Specialist function in place in the Trust. It should:
-
Receive the annual work plan and annual report.
-
Ensure the independence of the function.
-
Ensure that the function is adequately resourced.
-
Consider findings derived from both internal cases and any national initiatives.
-
Receiving a report of all cases involving fraud
-
Losses and Special Payments
-
By virtue of Standing Financial Instruction (SFI) 14.2 the Chief Financial Officer must prepare procedural instructions on the recording of and accounting for condemnations, losses, and special payments. The Committee shall monitor this function by reviewing the Trust’s Register of Losses and Special Payments.
Financial Reporting
-
The Committee shall monitor the integrity of the financial statements of the Trust, and any formal announcements relating to the Trust’s financial performance, reviewing significant financial reporting judgements contained in them.
-
This will be achieved by reviewing the Annual Report and Financial Statements before submission to the Board, focusing particularly on:
-
The wording in the Annual Governance Statement and other disclosures relevant to the terms of reference of the Committee
-
Changes in, and compliance with, accounting policies and practices
-
Unadjusted mis‐statements in the financial statements
-
Major judgmental areas
-
Significant adjustments resulting from the audit
-
Compliance with the NHS Foundation Trust Financial Reporting Manual
-
-
The Committee should recommend to the Board as to whether the annual financial statements should be adopted by the Board.
-
The Committee ensure that the systems for financial reporting to the Board, including those of budgetary control, are subject to review as to completeness and accuracy of the
information provided to the Board.
Accounting Policies
-
To review, approve and keep up‐to‐date accounting policies of the Trust to ensure that they are fit‐for‐purpose for an NHS Foundation Trust.
Other assurance functions
-
The committee shall review the findings of other significant assurance functions, both internal and external to the organisation and consider the implications for the governance of the organisation. These will include, but not limited to any reviews by regulators, professional bodies, accreditation bodies etc.
-
The Committee will review the work of clinical risk management the committee will wish to satisfy itself on the assurance that can be gained from the clinical audit function.
-
The Committee shall review the adequacy and security of the whistleblowing arrangements; that these arrangements allow proportionate and independent investigation and appropriate follow up action.
Documentation dealing with probity
-
To review comprehensiveness of documents dealing with probity including Standing Financial Instructions, Standing Orders, Standards of Business Conduct and Counter Fraud.
-
To update such documents in line with Department of Health guidelines and recommendations.
-
The Committee shall review all Board decisions to suspend Standing Orders, in accordance with SO s3.8.8.
-
The Committee shall review all waivers of Standing Orders in respect of competitive quotation and tendering procedures.
-
ACCOUNTABILITY & REPORTING
-
The minutes of the Committee meetings shall be formally recorded and available to the Board of Directors.
-
The Committee shall receive the Chair’s Reports of the other three Board Committees - Quality Assurance Committee, People and Remuneration Committee, Performance and Finance Committee as part of ensuring the maintenance of an effective system of integrated governance.
-
The Chair of the Committee shall draw to the attention of the Board any issues that require disclosure to the full Board or require executive action.
-
In particular, the Chair of the Committee shall disclose any evidence of ultra vires transactions or improper acts to the Board, in accordance with SFI s2.1.2.
-
The Committee shall also report to the Council of Governors, as required, identifying any matters in respect of which it considers that action or improvement is needed and making recommendations as to the steps to be taken.
-
The Committee will report to the Board annually on its work in support of the Annual
-
Governance Statement, in advance of the Board meeting to agree the Annual Report and Accounts.
-
COMMITTEE SECRETARY
-
The Committee will be supported administratively by the Committee Secretary, whose duties in this respect will include:
-
Agreement of agenda with Chair and attendees and collation of papers.
-
Taking the minutes and keeping a record of matters arising and issues to be carried forward.
-
Advising the Committee on pertinent areas.
-
Under the direction of the Chair, drafting the Committee’s annual report.
-
Keeping a record of attendance at meetings.
-
-
The Trust Secretary will ensure that these terms of reference are compliant with NHS Resolution risk management standards and monitor compliance with the standards.
-
-
Review
Date Approved: 2nd July 2019 Review: 1st September 2020 Review: 9th September 2021 Review: 2nd September 2022 Review: 8th November 2023
Strategic Objective 2 – Exceptional care
Risk Description 2.4 Risk that governance systems fail to identify and address areas of risk and concern. Risk Appetite – the Trust has a low/averse appetite for risks that impact on governance
Date last reviewed:
November 2023
Director Lead:
Caroline Donovan, CEO
Board Committee:
Audit & Risk Committee
Consequence of risk:
If governance systems fail, then this impacts on quality and safety of care, patient outcomes, CQC rating, failure to exit Recovery Support Programme (RSP)
Target Rating: (l x c) and Date to reach target
2 x 4 = 4 March 2024
Risk Rating over time
30
25
20
15
10
5
0
Rationale for current score: (l x c) Improving local governance and improving data quality and governance supporting
learning from deaths, hence increased rating
Jan-23 Mar-23 May-23 Jul-23 Sep-23 Nov-23
Controls (what are we currently doing about the risk?)
-
Improvement programme – focus on improving local governance and learning from deaths as part of Quality & Safety pillar
-
Strengthened board and committee level governance; annual review underway, ensuring floor to board reporting and assurance
-
Continuing to improve QPMs and care group governance. NED attendance at QPMs
-
Accountability Framework and Leadership Competency Framework (LCF) in place, but work on going to strengthen and embed
-
Risk Management framework, policy and strategy undergoing annual review. New Board Assurance Framework linked to new Trust Strategy. Continued Corporate Risk Register scrutiny. New local risk register process launched
-
Standing Financial Instructions across N&W ICB.
-
NHSE and system performance meetings (OAG)
-
Evidence Assurance Group scrutinises CQC must evidence, chaired by N&W CMO) and New Recovery Support Group (RSP) established, chaired by NED, to do the same with RSP criteria
Assurances (how do we know if the things we are doing are having impact?)
-
Improvements highlighted by CQC report published February 2023, although Trust remains in RSP. Improvement Board monitoring progress with Improvement programme, CQC must dos
-
Executive and NED scrutiny and challenge of each improvement pillar work
-
Evidence Assurance Group signing off CQC must do evidence – on track
-
Local Governance Delivery Group with support from NHSE. Escalating issues with recruitment for key lead post to drive programme at pace. Good progress with roll out of MEG software for audits and early warning trigger tool
-
Performance & Finance Committee November discussing QPM effectiveness
-
IQPR metrics – yet to show sustainable improvement and reflect ‘so what’ aspect of impact on service users, carers, staff
-
Internal Audit of BAF May 2023 and Assurance mapping July – both ‘reasonable assurance’ opinion – actions underway to address recommendations.
-
Overdue risks remain on Corporate Risk Register – comply or explain approach by A&RC, along with programme of BAF risk check and challenge with exec and NED lead for each risk. Each Board committee scrutinises relevant BAF risks and high rated corporate register risks. Nov A&RC escalated concerns re timely updating of risks – now has a KPI on the improvement programme outcomes dashboard
|
evidence. Reporting to Improvement Board and Audit & Risk Committee (A&RC) respectively |
|
|---|---|
Gaps
| Mitigating actions (what more should we do?)
|
|
Report To: |
Board of Directors |
|---|---|
Meeting Date: | 23rd November 2023 |
Title of Report: | Quality Assurance Committee (QAC) Chairs’ Report |
Purpose of report: | For Assurance |
Authors: | Roger Hall, Non-Executive Director |
Director: | Zoe Billingham, Chairperson |
Link to Trust Strategy | Links to all Strategic objectives |
Legislation / compliance | CQC Well-Led; NHSE performance framework |
Link to BAF / Risks | All risks on Board Assurance Framework as each Committee reviews those relevant to its terms of reference |
Executive Summary:
This report provides an update to the Board on the meeting of the Quality Assurance Committee (QAC) held on 13th November 2023, via MS Teams.
Recommendation
The Board is asked to note the report.
Quality Assurance Committee Chair’s Report – 13th November 2023
The committee was disappointed with the late submission of papers and strongly encouraged a rapid return to timely submission.
Decisions taken
The following annual reports were approved and commended for submission to the Board:
-
Annual Safeguarding Report
-
Infection Prevention and Control Report
-
Research and Development Annual Report
Assurance received
1/ Safeguarding training for doctors
A paper was received outlining steps being taken to improve the poor reported compliance for level 3 training in both adult and children's safeguarding for doctors. Assurance was received about additional training opportunities for doctors that would be delivered face to face locally. What remains unclear is the trajectory towards compliance; the committee requested a plan that would assure it that the current plans were sufficient to achieve compliance in a reasonable timeframe.
There remains data quality issues related to meaningful capturing of training achievement; compliance is measured annually but the training is delivered over 3 years.
2/ Learning from deaths
Strong assurance was received in the Learning from Deaths Report in the following areas:
a/ The definition of deaths and the appropriate mechanism (including Trust Governance) for reviewing each category
b/ Progress with improving mortality data collection is satisfactory with the new daily (previously monthly) collection going live in early November. The improved system will allow greater correlation of deaths with other systems for example demographic data associated with deprivation.
Care Group Presentation
A comprehensive update was received from Rollesby Ward. The committee was pleased to hear about the principles of Psychiatric Intensive Care Units and that these were being adhered to in the ward. We were also guided through likely demand patterns and were pleased that even although there have been staffing stresses in Rollesby demand had been met safely to date. A concern was raised about the possibilty that the ward might in the future be used to care for lower acuity patients which would make it difficult to provide the right environment for both higher and lower acuity patients.
Research and Development
The committee received the annual R & D report which provided an excellent summary of research activity in the Trust. It was clear that R & D is performing at a very high level; metrics including grant income, study recruitment and peer reviewed publications support this assessment. It is to be particularly noted that R & D is entirely self-funded with no recourse to Trust funding. The committee believes that, given the high performance of R & D greater emphasis of its role within the Trust's strategy will be required. Particular issues that ought to be reviewed by the Board include the possibility of pump priming funding, support for a Clinical Research Facility (likely to be income generating), wider publicity of research success and explicit allocation of funds such as PAs for research already designated for SPAs and through external funders such as HEE.
Quality and Safety Pillars
Both the Quality and Model of Care Pillar projects are on track with progress in appointing to key leadership positions in each pillar. The next QAC will receive a detailed paper on the Model of Care which will include examining efficacy of clinical outcome measures and how these change during treatment episodes (clinical effectiveness).
Board Assurance Framework (BAF)
The Committee’s two risks were reviewed. It was noted that Risk 2.1 was relatively silent on risk to those waiting for trust services and that as a consequence there were few mitigations. This will be reviewed.
The committee’s Corporate Risks were noted to be consistently high and, in many cases, inappropriately over scored. The scores will be reviewed.
Concern to be escalated to the Board
Previous QAC meetings have noted while reviewing the IQPR that it has been difficult to properly integrate areas that are currently reviewed by three separate committees of the Board (QAC, People and Performance). Discussion about issues such as waiting times for assessment and treatment particularly for children and young people in some services remains trapped as a descriptive process rather than focussed on improvement. The committee speculates that important cross cutting issues such as waiting times with complex interplay between staffing, operational performance and quality need to be considered by the entire Board to drive improvement.
Strategic Objective 2 – Exceptional care
Risk Description 2.1 Risk of failure to deliver high standards of quality, safety and effectiveness. Risk Appetite – the Trust has a very low/averse appetite for risks that impact on quality, safety and patient experience
Date last reviewed:
November 2023
Director Lead:
Tumi Banda, Interim Chief Nurse. Alex Lewis, CMO
Board Committee:
Quality Assurance Committee (QAC)
Consequence of risk:
If the Trust fails to deliver high quality, safe effective services, this impacts on service user outcomes, confidence and trust by the public, poor CQC ratings and continuation in Recovery Support Programme and poor staff morale and retention.
Target Rating: (l x c) and Date to reach target
3 x 4 = 12 once must dos addressed as ascertained by next
Risk Rating over time
25
15
5
Rationale for current score: (l x c) Progress, but yet to fully address the CQC concerns as per quality and safety metrics
CQC inspection
Controls (what are we currently doing about the risk?)
-5 Jan-23 Mar-23 May-23 Jul-23 Sep-23 Nov-23
Assurances (how do we know if the things we are doing are having impact?)
-
Daily and weekly huddles focused on safety and quality matters - from clinical teams to the executive
-
The NHSE Patient Safety Strategy and incident investigation Framework review processes following incidents, is embedding within the Trust, with regular patient safety incident reporting. The Strategy priorities including implementation of PSIRF, Safety Culture, addressing national patient safety alerts, undertaking patient safety training and working towards safety improvement are all in progress or complete.
-
Safe staffing controls –Roster Check & Challenge meetings are continuing every 4 weeks to monitor inpatient roster performance & to scrutinise rostering KPI’s
-
Supervision, Appraisals, Mandatory Training.
-
Clinical Guidance via policy and operational procedures.
-
Application of NHSE Patient Safety Framework including incident reporting system.
-
Availability of multiple routes for staff to raise query and concern.
-
Triangulation of quality outcomes with feedback from experience from carers and patients (e.g., Friends and Family Test, Complaints, People Participation Team) to receive and act upon user and carer feedback. Reported to Quality Assurance Committee, Experience of Care, QPM
-
Integrated Quality Performance Report (IQPR) quality & safety metrics, reported to QAC and Board shows: nil never events and no prevention of future death notifications this period. Reduction in ligature incidents using a fixed point. Reduction in restrictive practice (prone restraint, rapid tranquilisation). Supervision (October decline by 3% to 69%), Appraisals (October increase by 3% to 84%), Mandatory Training (October increase by 1% to 89%) below target.
-
Roster data shows continued improvement for day and night fill rates, majority above target levels of 90%.
-
Utilisation of feedback from customer services, use of the Family and Friends to inform on quality and experience of patients and carers monitored by Experience of Care Committee
-
Triangulation with feedback from range of sources including Quality & Safety reviews which provides ongoing assessment against standards with action plans to improve
-
Clinical Audit Programme, approved by QAC and A&RC, reporting on themes to Quality Committee
-
Evidence Assurance Group (EAG) have signed off Must Do actions according to plan
-
Oversight of MEG audits reviewed in relevant committees, and included within EAG templates
|
|
|---|---|
Gaps
| Mitigating actions (what more should we do?)
and improvement Board. |
Safewards; Early Warning Trigger Tool. |
|---|
|
Strategic Objective 2 – Exceptional care |
|||
|---|---|---|---|
Risk Description 2.2 Risk of failure to acquire and record accurate data on deaths and Serious Incidents will compromise learning and delivery of safe services. Risk Appetite – the Trust has a very low/averse appetite for risks that impact on quality, safety and patient experience | Date last reviewed: November 2023 | Director Lead: Alex Lewis, CMO Tumi Banda, CN | Board Committee: Quality Assurance Committee |
Consequence of risk: If the Trust fails to acquire and record accurate data on deaths and serious incidents then these compromises learning and prevention, delivery of safe services and working with partners to reduce inequalities in health care | Risk Rating over time 25 20 15 10 5 0 Jan-23 Mar-23 May-23 Jul-23 Sep-23 Nov-23 | Rationale for current score: (l x c) Progress with action plan following the Grant Thornton mortality report High Risk 4 x 4 = 16 | |
Target Rating: (l x c) and Date to reach target 3 x 4 = 12 March 2024 | |||
Controls (what are we currently doing about the risk?)
Standard Operating Policy outlines processes, assurance and evaluation | Assurances (how do we know if the things we are doing are having impact?)
dashboard, and ICB learning from deaths forum |
|
including engagement with Clinical Experts and ICB colleagues to decide on safety activity and actions
Monday |
|
|---|
|
Gaps (in controls and assurances)
including premature death |
Mitigating actions (what have we done/what more should we do?)
|
|---|
Integrated Quality and Performance Report
Version for Trust Board Submitted 15th November 2023
|
Section |
Page |
|---|---|
| 3 – 12 | |
| 13 – 22 | |
| 23 – 30 | |
| 31 – 38 | |
| 39 – 46 | |
41 | |
42 | |
| 43 – 47 |
Integrated Quality and Performance Report
Operational Performance Period to end September 2023






 Operational Performance Summary
Operational Performance Summary

 Will
consistently pass the target if nothing changes
Will
consistently pass the target if nothing changes
Will not consistently pass or fail the target if nothing changes
Assurance
Will consistently fail the target if nothing changes
No target
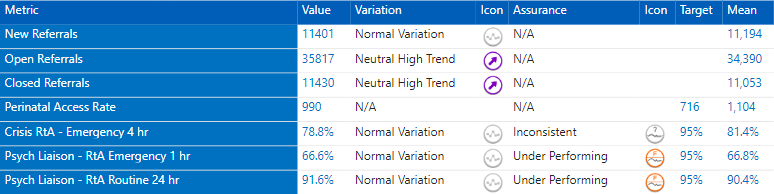




*(formerly IAPT)
 Working
together for
Working
together for
better mental health Integrated Quality & Performance Report Latest data from September 2023
Page 6











Working together for
Page 12
Integrated Quality and Performance Report
Quality & Safety
Period to end September 2023
Working together for







 Quality & Safety Performance Summary
Quality & Safety Performance Summary








Quality & Safety | Incident Reporting

Quality & Safety | Self Harm and AWOL

Quality & Safety | Assaults and Falls




Integrated Quality and Performance Report
Workforce
Period to end September 2023









 Workforce Performance Summary
Workforce Performance Summary

 Workforce | Executive Summary
Workforce | Executive Summary
 Safer Staffing
Safer Staffing
Summary:
-
Safer Staffing levels and fill-rates continue to be monitored across all inpatient units to ensure safety & consistency.
-
Agency staffing costs have decreased year on year
-
Long Term Agency Placements – all new LTP's are now being scrutinised at FRP each week
-
SafeCare; acuity input compliance hit its highest level in Sept at 91.85%. Additional clinical training being sought by NHSE.
Priority Actions:
-
Staffing Establishment reviews completed in all inpatient areas, findings being reviewed.
-
Roster Check & Challenge meetings are continuing every 4 weeks to monitor inpatient roster performance & to scrutinise rostering KPI’s
-
Temporary staffing controls; additional measures in place for senior approval for staffing numbers to increase above standard levels
-
To maintain consistency of SafeCare compliance levels
Workforce | Sickness Absence



 Workforce | Safer Staffing
Workforce | Safer Staffing
Integrated Quality and Performance Report
Financial Performance 2023/24 Month 7 – October 2023
Executive Summary M7 (October 2023)
This paper reports financial performance as at 31 October 2023 (M7).
Trustwide performance: The retained YTD position was a £4.8m deficit, in line with plan.
The 2023/24 financial plan is a full year break-even position, this remains forecast to be delivered, albeit with significant non-recurrent mitigations required.
Without non-recurrent mitigations the Trust’s underlying deficit is currently c.£12.8m. Significant interventions are required to deliver an exit run rate which is sustainable moving into future financial years.
The efficiency programme is forecast to deliver £2.5m of recurrent schemes against planned levels of £9.0m. The shortfall is being mitigated by non- recurrent delivery, however, as noted above this will impact future years sustainability.
Drivers of the position: Care Services are reporting a net operational deficit of
£6.2m including COO efficiency target. The YTD underlying overspend of
£10.7m is mitigated by the £3.1m non-recurrent mitigation and £1.4 over- delivery of non-recurrent efficiencies against the recurrent efficiency target. The full year net operational deficit is forecast to be £16.6m without intervention.
Within the Care Services operational deficit, Out of Trust (OOT) placements, including PICU spend, was £0.4m adverse to plan for the month and £2.6m adverse YTD.
YTD there have been 2,590 days of Delayed Transfers of Care (DTOC) which equates to a cost pressure of £1.8m, and is forecast to be £2.6m if the October levels continue for the remainder of the year.
Other items: Cash held by the Trust at 31 October was £38.5m, which was
£5.3m ahead of plan, predominately due to the under spend on the capital programme YTD and also NHSE LDA funding received in advance.
Capital expenditure is behind the original plan due to the change in the Rivers
Centre spend profile which has been agreed with the system partners, excluding this adjustment the capital plan is forecast to be in line with plan.
The N&W ICS remains reporting on plan for its FOT, however, significant risk is within this position due to the uncertainty regarding the impact of strike action on the Elective Recovery Funding (ERF). SNEE ICS is reporting a deficit position for the same reasons.
Next steps: The Trust is formulating a financial special measures regime to develop recovery plans for the areas overspending, and the implementation of additional internal controls, to ensure the Trust meets the 2023/24 financial plan.
Close monitoring of OOT performance against trajectory with a revised trajectory required and mitigations identified for the risk to delivery has been identified.
Increased focus on the delivery of the recurrent efficiency targets to move the exit run rate to a sustainable level.
 Working
together for
Working
together for
better mental health Integrated Quality & Performance Report Latest data from September 2023
Page 32

 Financial Summary Month 7 (October 2023)
Financial Summary Month 7 (October 2023)

 Forecast Outturn & Underlying Deficit Month 7 (October 2023)
Forecast Outturn & Underlying Deficit Month 7 (October 2023)

 Efficiencies Month 7 (October 2023)
Efficiencies Month 7 (October 2023)
|
FOT performance There has been a £0.3m negative movement in month, relating to £0.4m Hellesdon Upper Plateau depreciation savings not now being achievable in year, partly offset by a £0.1m improvement in Pharmacy drug switch schemes Recurrent v Non-Recurrent FOT The original plan showed a plan of £9m recurrent and £4m non- recurrent. The current position has significantly deteriorated to a mix of £2.5m recurrent and £10.5m non-recurrent. This will have a significant impact on the Trusts’ ability to breakeven in the 2024/25 financial year. Full Year Effect The full year effect of this years schemes is now predicted at £4.0m, with the reduction due to the Hellesdon Upper plateau changes. However, it is worth noting that there are a number of schemes which have not commenced yet which would significantly improve the full year effect position. Examples of these schemes are ‘Long term vacancies review’ and ‘Review of ward and community admin’. |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
|
YTD FULL YEAR FULL YEAR EFFECT |
|||||||||
|
Department |
Actual | Plan |
Var - Fav/(Adv) |
FOT |
Plan |
Var - Fav/(Adv) |
FOT |
Plan |
|
| £m's | £m's |
£m's |
£m's |
£m's |
£m's |
£m's |
£m's |
£m's |
|
|
Recurrent |
1.0 | 2.5 |
(1.5) |
2.5 |
9.0 |
(6.5) |
4.0 |
13.0 |
(9.0) |
|
Non-Recurrent |
6.8 | 2.3 |
4.5 |
10.5 |
4.0 |
6.5 |
0.0 |
0.0 |
0.0 |
|
Total |
7.8 | 4.8 |
3.0 |
13.0 |
13.0 |
0.0 |
4.0 |
13.0 | (9.0) |
Statement of Financial Position Month 7 (October 2023)

 Statement of Financial Position Month 7 (October 2023) – (continued)
Statement of Financial Position Month 7 (October 2023) – (continued)
Financial Risks Month 7 (October 2023)
 Likelihood
Likelihood
|
KEY TO BOX COLOUR |
|---|
Increased risk in month No change to risk in month Reduced risk in month |
Integrated Quality and Performance Report
Appendices
Appendix 1 - What is an SPC Chart?

 Appendix 2 - SPC Chart Icons
Appendix 2 - SPC Chart Icons
|
Metric ID |
Metric |
Definition |
Methodology/Exclusions |
Data source |
|---|---|---|---|---|
OP54 | New Referrals | New internal and external referrals into NSFT in monthly | The number of new referrals into the trust during the reported period split then by priority. | Lorenzo |
OP61 | Crisis RtA - Emergency 4 hr | Percentage of crisis team referral-to-treatment eligible emergency episodes with first attended assessment contact in monthly period that were assessed within four hours, split by age (under 18 and 18 and over) |
| |
OP61a | U18 Crisis RtA - Emergency 4 hr | |||
OP61b | 18+ Crisis RtA - Emergency 4 hr | |||
OP28 | Psych Liaison - RtA Emergency 1 hr | Percentage of emergency referrals to the psychiatric liaison service with first face-to-face attended contact in monthly period that were within one hour of the referral start time |
| |
OP29 | Psych Liaison - RtA Routine 24 hr | Percentage of routine referrals to the psychiatric liaison service with first face-to-face contact in monthly period that were within 24 hours of the referral start time | ||
OP12 | RtA - Routine 28 days | Percentage of referral-to-treatment eligible non- emergency episodes with first attended assessment contact in monthly period that were assessed within 28 days, split by age (under 18 and 18 and over) at the date of the RTT eligible spell commencing |
| |
OP12a | U18 RtA - Routine 28 days | |||
OP12b | 18+ RtA - Routine 28 days | |||
OP01 | EIP Access & Wait Time Standard | Percentage of referrals into and within NSFT with suspected first episode psychosis or at 'risk mental state' that start a NICE-recommended care package in monthly period that were within two weeks of referral |
| |
OP13 | RtT within standard | Percentage of referral-to-treatment eligible episodes with first attended treatment contact in monthly period that were treated within the standard (Norfolk & Waveney = 18 weeks, Suffolk = 15 weeks), split by age (under 18 and 18 and over) at the date of the RTT eligible spell commencing and service line (Adult Community Service Team, DCLL Service Team, and CFYP Service Team) |
| |
OP13a | U18 RtT within standard | |||
OP13b | 18+ RtT within standard | |||
OP13b(i) | Adult Community - 18+ RtT within standard | |||
OP13b(ii) | Dementia/Later Life - 18+ RtT within standard | |||
OP13b(iii) | CFYP - 18+ RtT within standard |
|
Metric ID |
Metric |
Definition |
Methodology/Exclusions |
Data source |
|---|---|---|---|---|
OP15 | U19 Eating Disorders - RtT Urgent 1 wk | Percentage of CYP with a suspected eating disorder for urgent cases starting teatment in monthly period that started treatment within one week of referral |
| Lorenzo |
OP16 | U19 Eating Disorders - RtT Routine 4 wk | Percentage of CYP with a suspected eating disorder for routine cases starting teatment in monthly period that started treatment within four weeks of referral | ||
OP10 | Access | Total access to IAPT services | ||
OP07 | 6 week wait | Number of patients who waited less than or equal to 6 weeks for their first treatment contact | ||
OP08 | 18 week wait | Number of patients who waited less than or equal to 18 weeks for their first treatment contact | ||
OP06 | Recovery | The proportion of people who are moving to recovery | ||
OP57 | Inpatient Admissions | Inpatient admission in monthly period | The number of patients admitted to an inpatient ward during reported period. | Lorenzo |
OP58 | Inpatient Discharges | Inpatient discharges in monthly period | The number of patients discharged from an inpatient ward during reported period. | |
OP20 | Delayed Transfer of Care (DToC) | Percentage of consultant-led and non-consultant-led occupied bed days in monthly period including delayed transfers of care attributable to social care services that were non-acute patients aged 18 and over on admission whose transfer of care was delayed | DToC Clock start: As soon as an adult patient meets these three conditions and remains in hospital
| |
OP09 | Inappropriate OAPs - bed days | Total number of inappropriate out of area placement bed days in adult mental health services. | An OAP will be inappropriate if the reason is non-availability of a local bed. An out of area placement may be appropriate when, e.g. (not an exhaustive list):
|
|
Metric ID |
Metric |
Definition |
Methodology/Exclusions |
Data source |
|---|---|---|---|---|
OP60 | 72 hour follow up | Percentage of people under adult mental illness specialties discharged from psychiatric inpatient care that were followed up within 72 hours |
The following excludes from the metric;
| Lorenzo |
OP21 | Inpatients with annual PH check | Percentage of inpatients with a length of stay exceeding 12 months at the end of the monthly period that received an annual health check within the previous 12 months | Presence of a finalised annual health check form with assessment date within the previous 12 months. Exclusions
|
|
Metric ID |
Metric |
Definition |
Methodology/Exclusions |
Data source |
|---|---|---|---|---|
WF01 | Annualised Sickness absence % | Full-time equivalent (FTE) calendar days lost to sickness absence in a rolling 12-month period, expressed as a percentage of available FTE calendar days lost in the same 12-month period | All substantive staff included | Electronic Staff Record |
WF02 | In Month Total Sickness Absence Rate % | Full-time equivalent (FTE) calendar days lost to sickness absence in a month period, expressed as a percentage of available FTE calendar days lost in the same month period | ||
WF02a | In Month Total Sickness Absence Rate % (Short Term Sickness) | Full-time equivalent (FTE) calendar days lost to short-term sickness absence (episodes lasting 27 days or less) in a month period, expressed as a percentage of available FTE calendar days lost in the same month period | ||
WF02b | In Month Total Sickness Absence Rate % (Long Term Sickness) | Full-time equivalent (FTE) calendar days lost to long-term sickness absence (episodes lasting 28 days or more) in a month period, expressed as a percentage of available FTE calendar days lost in the same month period | ||
WF03 | % of time lost to stress/anxiety/depression | Full-time equivalent (FTE) calendar days lost to sickness episodes relating to stress/anxiety and depression in a month period, expressed as a percentage of available FTE calendar days lost in the same month period | ||
WF12 | Substantive Staff at the end of month | Count of full-time equivalent staff at end of Month | ||
WF04 | In Month Overall Vacancy Rate % | The difference between establishment and contracted staff in post | All funded posts included | Integra |
WF05 | All Staff Turnover % | All leavers divided by the average staff in post over the previous 12 months (includes fixed-term, locum and bank leavers) | The term ‘all turnover’ is used to encompass all leavers, both voluntary and involuntary, including those who resign, retire or are made redundant | Electronic Staff Record |
WF17 | % Voluntary Leavers not completing 2 years service | Voluntary leavers not completing 2 years' service divided by the total number of voluntary leavers | None | |
WF08 | Management Supervision | Percentage of staff with a current valid period of management supervision | All management supervision recorded on ESR, excluding staff on maternity leave, long-term sickness absence and staff who have completed less that one month's service | |
WF09a | % Total Appraisal Rate (Non-medical Staff) | Percentage of non-medical staff with a completed appraisal within a rolling 15-month period | All appraisals recorded on ESR, excluding staff on maternity leave, long- term sickness absence and staff who have completed less that 12 | |
WF09b | % Total Appraisal Rate (Medical Staff) | Percentage of medical staff with a completed appraisal within a rolling 15-month period | ||
WF10 | % Mandatory Training Completed | Percentage of mandatory/statutory and essential training items completed, against all mandatory/statutory and essential training items | All mandatory training items recorded on ESR, excluding staff on maternity leave, long-term sickness absence and staff who have completed less that three months' service | |
WF11a | Day Time Average shift fill rate - registered nurses (%) | Total worked monthly day registered nursing staff hours versus planned day registered nursing staff hours | Covers inpatient ward areas only | NHSP/Health Roster |
WF13a | Day Time Bank/Agency registered nurses (%) | Agency and bank hours worked at day time by registered nurses divided by the total day registered nurse actual hours worked | ||
WF11b | Day Time Average shift fill rate - care staff (%) | total worked monthly day care staff hours versus planned day care staff hours | ||
WF13b | Day Time Bank/Agency Care Staff (%) | Agency and bank hours worked at day time by care staff divided by the total day care staff actual hours worked | ||
WF11c | Night Time Average shift fill rate - registered nurses (%) | Total worked monthly night registered nursing staff hours versus planned night registered nursing staff hours | ||
WF13c | Night Time Bank/Agency registered nurses (%) | Agency and bank hours worked at night time by registered nurses divided by the total night registered nurse actual hours worked | ||
WF11d | Night Time Average shift fill rate - care staff (%) | Total worked monthly night care staff hours versus planned night care staff hours | ||
WF13d | Night Time Bank/Agency Care Staff (%) | Agency and bank hours worked at night time by care staff divided by the total night care staff actual hours |
01603 421421
nsft.nhs.uk @NSFTtweets NSFTrust
|
Report to: |
Board of Directors |
|---|---|
Meeting date: | 23rd November 2023 |
Title of report: | Learning from Deaths Report April 2022 – September 2023 |
Purpose of paper: | For information and assurance |
Author: | Dr Uju Ugochukwu – Medical Director for Quality |
Director: | Dr Alex Lewis - Chief Medical Officer & Tumi Banda - Chief Nurse |
Regulation/ Compliance | NHSE and CQC regulations |
Link to Trust Strategy | Delivering exceptional care |
Executive summary
The paper provides an update on how the Trust is responding to the NHSE’s Patient Safety Strategy (2019). It outlines additional requirements from the Learning from Deaths programme to ensure that all deaths are scrutinised independently through the Medical Examiner System.
The report offers information and improvements to ensure NSFT comply with statutory expectations against the Learning from Deaths guidance and wider mortality activities, governance, and assurance. It provides an update on the external review completed by Grant Thornton UK LLP on the collection, processing and reporting of data related to patients’ deaths at NSFT.
Recommendation
The Committee is asked to consider the information and updates provided in this report.
Learning from Deaths
-
Introduction/Background
-
The expectations in relation to reporting, monitoring and Board oversight of mortality incidents are set out in the National Quality Board’s ‘Learning from Deaths’ guidance (March 2017), and builds on the recommendations made by the Mazars investigation into Southern Health (Dec 2015), the CQC report ‘Learning, Candour and Accountability publication’ (Dec 2016) and the Learning Disabilities Mortality Review (LeDeR) which is managed by NHS England. The Learning from Deaths framework (LfD) places particular responsibility on Trust Boards to ensure their trust has robust systems for recognising, reporting, and reviewing or investigating deaths where appropriate. The Learning from Deaths (LfD) states ‘the aim of this process is to ensure that all deaths of people under the Trust’s care are reviewed at the appropriate level and organisational learning occurs’.
-
The Patient Safety and Incidents Framework (PSIRF) focuses on incidents of unexpected and unnatural deaths related to acts or omissions in care that may have contributed to the death of a patient. Whereas the Mortality process focuses on learning when people have died from expected/
unexpected natural causes and where no patient safety incident has been identified.
-
Mortality Scrutiny
-
The current Learning from Deaths process Learning from Deaths led by the Patient Safety team ensures that all death notifications are reported through the trust incident safety system (Datix) and NHS Spine. Initially the primary consideration made by the Patient Safety Team is whether the death meets the criteria for report and investigation under Policy Q11 Serious Incidents Requiring Investigation. Deaths not investigated under Policy Q11 Serious Incidents requiring Investigation will be in scope for review using the mortality review process (Mortality Team).
-
A dedicated mortality team is now in place to oversee Mortality, and the implementation and ongoing management of the Medical Examiner system. The team comprises of a Clinical Lead, and a data analyst together with a Mortality Lead to oversee the process.
-
The role of the Mortality Team is to screen all deaths (NHS Spine, Datix and Medical Examiners) and follow the system of consideration of further investigation/ review as detailed in the mortality process and case selection criteria.
-
The monthly Learning from Deaths and Incidents Committee (previously the Safety and Mortality Committee) chaired by the Medical Director for Quality has a new Terms of Reference and Workplan and is attended by the Clinical Leads from each Care Group, the Head of Carers Participation and Experience, People Participation Lead and the Advisor for Suicide Prevention and Lived Experience. The ICBs from Norfolk and Suffolk are both represented. The committee leads on the analysis of the reported data to identify recommendations from mortality reviews. This is based on a range of factors including age groups, causes of death, clinical and geographical areas, and deprivation scores. In addition, the committee commission Mortality reviews where themes/ patterns are identified. The committee reports to the Quality Committee, the Quality Assurance Committee and to the Trust Board quarterly.
The Mortality Scrutiny Group, commenced in June 2023 is supported by a range of clinicians and practitioners from different disciplines and organisations. This group scrutinises the learning from all mortality reports and mortality data from the dashboard to make recommendations for focused local and strategic improvements. The Mortality Scrutiny Group will report to the Learning from Deaths Committee, submitting a themes and trends report and provide the data and learning to the Trust Physical Health committee on a quarterly basis.
-
Seagry Consultancy company were commissioned by the Trust in April 2023 to assist in the improvement of processes and systems that support the production of mortality reporting.
-
Mortality Process focuses on learning from natural cause deaths, both expected and unexpected. Its aim is to enable mental health trusts to work alongside other trusts and organisations to improve the physical health care provision for people with severe and enduring mental illness (SMI), autism, and/ or a learning disability.
Mortality for mental health trusts became an NHS priority as a response to The Five Year Forward View for Mental Health (NHSE 2016), where it was identified that people with severe and prolonged mental illness are at risk of dying on average 15-20 years earlier than other people. Thus, the health inequalities present for people with severe mental health issues and learning disabilities, is the focus. In 2021, NHS E included in scope people with autism.
The guidance from the National Quality Board makes it clear that trusts should report on inpatient deaths and those inpatients that have died within 30 days of leaving hospital. Locally, trusts determine their own individual approaches to undertaking mortality reviews. As mandated, the trust complete reviews for all patients who have died whilst they are an inpatient (the same as acute general care). However, as a community mental health trust, there are additional responsibilities.
This includes reviews of people’s care that die in the community who experience serious mental illness, learning disability or autism (NHSE Learning from Deaths Mental Health). To determine which deaths are in scope for review, NSFT have utilised the original Serious Incident Framework (2015) guidance to include the deaths of all patients in receipt of care from the Trust and within six months of discharge.
Consequently, as trusts follow differing approaches as to who is included, mortality data is not comparable between Trusts. As such the Trust will continue to evolve processes and refine reporting over time in accordance with local and national learning. This is in addition to the detailed reporting and investigation of deaths meeting the national criteria and local priorities under the Patient Safety Incident Response Framework (PSIRF). To note, PSIRF has replaced the Serious Incident Framework (2015).
NHSE provide some guidance in relation to mortality for mental health trusts, however this is unspecific therefore the Mortality team (as with most other NHS mental health trusts) follow the Mazars Framework which was written to assist trusts in developing a case selection process for Structured Judgement Reviews.
For ease we have separated this guidance into the three main categories:
-
Natural Expected – e.g., person on end-of-life care
-
Natural Unexpected – e.g., cardiac arrest, stroke, diabetes
-
Unnatural Unexpected – deaths that potentially meet the Patient Safety Incident Response Framework Priorities e.g., all unexpected inpatient deaths, please see link to the Trust’s Patient Safety Incident Response Plan Patient Safety Incident Response Plan 2022-23
A Structured Judgement Review is designed specifically to learn from deaths that do not involve any patient safety concerns. NSFT utilise the Royal College of Psychiatrists Mortality Review Tool. The clinical records are reviewed by clinicians not involved in the patient’s care and focuses on the different phases of care and contact with services. This is to ensure that good care is recognised, judged and recorded in the same detail as problematic care; to provide information about what can be learned when care goes well, and to identify gaps, problems or difficulties in the care received by the patient.
-
Data Analysis - Mortality
-
The Grant Thornton review highlighted several areas in which the recording and reporting processes for Mortality data could be improved. A new process to address these issues was implemented on the 6th November 2023 and is currently in the ‘early life support’ phase of project delivery.
-
To understand the changes and the resulting benefits the two processes are outlined below. The ‘old’ process is shown in image 1.
-
Informatics supplied a monthly patient deaths report to the Patient Safety Team. This report was based on information downloaded from the Personal Demographics Service (PDS) via the
-
Service User Death Report (SUDR) sourced from the NHS Spine (which is the official means of notifying deaths through clinical systems).
-
The Patient Safety Team used the PDS report, as well as information on patient deaths that had been logged on Datix, to populate their mortality workbook. This workbook was also used to collect further information about the patient deaths. The mortality workbook was the source for all external and internal reporting on patient deaths.
 Image 1 – ‘old’ mortality reporting process (pre-Nov 23)
Image 1 – ‘old’ mortality reporting process (pre-Nov 23)
-
The revised process is shown in image 2. Information on patient death is now received daily from both the PDS report and the Trust’s EPR systems that directly interact with the NHS Spine. This is an automated process.
-
The mortality data is automatically pushed through into the Trust’s Data Warehouse which in turn will update a SharePoint list which both the Patient Safety Team and Mortality Team can use to populate further required information about the patient deaths.
-
We have also included a monthly trace of all known patients against the Demographic Batch Service (DBS), which acts as a ‘back-stop’ in case any patient deaths are not notified via the daily SUDR.
Image 2 – new mortality process (from Nov 23)

-
This new process addresses the highlighted issues as shown in table 1 below:
|
Old process |
New process |
Benefit of process change |
|---|---|---|
Mainly manual process | Largely automated process |
|
Two sources of data | Multiple sources of data |
|
Run monthly | Run daily |
|
Data in different places | Data within a single place |
|
Manual reporting | Automated reporting |
|
Limited process documentation | Standard Operating Procedures |
|
Limited audit control | Audit control |
|
-
Where automated processes remain, these are either necessary and have clear processes in place or, in the case of the monthly DBS trace, will be automated in due course.
-
During the current early life support window for the new process, we will continue to learn from the introduction of the new approach and anticipate that there will be further enhancements we can make. Any future refinements will be made through appropriate change control to provide a clear audit trail.
-
These improvements have been built around the requirement of the Learning from Deaths framework for both Patient Safety and Mortality Teams supported by dedicated training.
-
All mortality data related to our old process prior to the 1st November remains available in our Mortality workbook and can be reported on. Data from the 1st November onwards, which has been processed according to the new approach put live on the 6th November, is available in a live daily dashboard. Because the two datasets were subject to different processes the mortality programme board took the decision not to migrate the legacy data into the new dashboard, as the ‘old’ data would not translate into the new format without some further changes.
-
Because of this a full quarter of data, processed under the new approach, will not be available until April 2024, however in the meantime the live dashboard is available to view daily and reports can be created against the Mortality workbook if necessary.
-
The new system will automatically pull demographic information, including levels of deprivation. With a dedicated Mortality Team, the Trust is now receiving 80% response rate for causes of death and to improve this further, there is focus on specific GP practices.
-
The richness of information will allow the Trust, ICBs and clinical teams to understand where improvements need to be focused, e.g., 50-year-old males experiencing serious mental illness in Great Yarmouth with higher rates of heart disease than the average population. System workstreams may want to take a view on access to care, physical health monitoring, provision of health promotion, ability to have a healthy diet, housing, education, and work.
-
Learning and good practice from Structured Judgement reviews
-
Learning
-
A thematic review was carried out on completed SJR reports on expected deaths of people receiving end-of-life care. The themed review focused on Mental Capacity Act assessments, best interest decisions, involving people with lasting power of attorney and ReSPECT (recommended summary plan for emergency care and treatment) documentation, which is a plan of care utilised at the end of life in discussion with the service user, their family and other significant parties. A summary of the findings is as follows:
-
Formal Mental Capacity Act assessments had been completed or partially completed but there was no evidence of best interest assessment to assist staff and families with decision making. The Trust has updated our Care of the Dying Person Policy to specifically include guidance on the Mental Capacity Act and have employed a Mental Capacity Act lead. Progress on this action is being overseen by the Learning from Deaths Committee.
-
Staff need training in the medico-legal legislation that will assist in decision-making when providing end of life care which is going to be led by the new Mental Capacity Act Lead.
-
Four key policies are being reviewed and/or update completed: Care of the Dying, Mental Capacity Act and Best Interest Decisions, Health Records and Do Not Attempt Resuscitation.
In addition, learning from individual SJRs can be summarised as follows:
-
Falls Reduction workstream – Work underway Trust wide which includes review of the policy, multi-professional Falls Reduction Steering Group, developing links between Mortality and Physical Health Care Team and sharing learning with the ward team.
-
Clozapine policy to include clarity as to expectations of medical reviews, guidance on constipation for staff and service users and the development of a ‘Policy on a Page’ as quick reference guide.
-
Improvements in clinical documentation.
-
Ward – ensuring that the care is personalised, and this is demonstrated within the documentation with improvements led through a QI project.
-
Community - ensuring completion of timely assessment and care plans which incorporate social care needs. Team QI project underway with progress reviewed in November 2023.
-
Good Practice
-
An example of good practice was the care of a gentleman on an Older Person’s ward receiving end of life care. Following NICE (QS13) End of Life Care for Adults, he was provided with personalised package of care inclusive of family and responsive to his changing needs.
-
Patient safety incidents requiring investigation between April 2022 – September 2023 (this information relates to unexpected/unnatural deaths only)
In line with the Patient Safety Incident Investigation Framework within this reporting period the trust undertook full reviews of fifteen patient safety incident deaths (unexpected/unnatural cause); three of these related to inpatient deaths which due to the type of incident namely self-inflicted harm were reported on STEIS and fully reviewed. There was a further unexpected/unnatural death which occurred within an out of area inpatient unit, a self-inflicted injury whilst the service user was on planned leave, which the trust is assisting with but is being led by the provider (The Priory).
The remaining twelve investigations related to; one victim of a domestic homicide, and a further eleven where the person had died due to suspected suicide/self-injury or an untoward safety incident.
To date of the fifteen reviews eight have been completed and signed off through the Quality Standards panel, five of these made recommendations for improvement to systems and processes (see the findings and action section below), and five remain in progress within acceptable timescales (90days). Trust wide recommendations are monitored through standards panel, local actions are monitored by the patient safety team link practitioners. The number of overdue recommendations continues to show an improving trend, reducing. There are currently eight outstanding actions being monitored by the Director for Nursing and Patient Safety.
-
Actions taken following notification of death by the Patient Safety Team, PFDs, Coroner’s Verdict, Cause of Death and Demographics
The patient safety team undertook 197 screenings (all deaths of this nature are screened), completed five After Action Reviews, twenty-eight safety incident reviews, commissioned two thematic reviews and fifteen full patient safety incident reviews.
In the financial year 2022/23 and up to September 2023 the trust received three prevention of future deaths (regulation 28) notifications; all were for Norfolk patients. Two patients tragically died in 2020 and one in 2021. The concerns raised related to:
PFD 1 – oversight and management of medication within clinic rooms and the training of medical staff in the administration of resuscitation medication. In response the trust has undertaken a full review of medicines optimisation across the organisation and is reviewing training requirements for medical staff in respect of life support resuscitation. Current compliance assurance on medication optimisation audits is 95% trust wide, the area for improvement is the standard of sharing medicines information with service users and carers; this forms part of the overall medicines optimisation improvement plan.
PFD 2 – risk assessment pre and post leave for patients on inpatient units. In response the trust has ensured that the use of SBAR (situation, background, assessment, recommendation) across the organisation has been standardized to improve the handover of risks. Current compliance assurance in relation to s17 leave and risk assessment is 93% trust wide, the area for improvement is the recording of feedback on leave from the service user and carers, if applicable, within the patient record; the relevant ward Matrons are addressing this with oversight from the Lead Nurses.
PFD 3 – contemporaneous recording of therapeutic observations and assessment of physical health care needs on mental health acute wards. In response the trust rolled out extensive competency training and refreshed the therapeutic observations policy in co-production with service users.
Current compliance assurance in respect of all aspects of the MEG audit around observations is 87%, the area for improvement is the standard of observations being reflected in the service user’s recovery plan; the relevant ward Matrons are addressing this with oversight from the Lead Nurses. Physical health monitoring compliance assurance is at 78% trust wide, areas for improvement cover multiple standards; the Director of nursing, physical health and IPAC, and the Medical Director for Quality have formulated an action plan to improve compliance in this area.
Up to 31st September 2023 there had been thirty- nine inquests related to service users known to the trust who have died by unexpected/unnatural means associated with a potentially harmful event or act. In respect of the confirmed suicide or narrative verdict “took own life” finding, there have been fifteen people confirmed as such at inquest up to 31st September 2023.



Age and gender; the majority of service users who died were male, aged between 41 – 60yrs of white British ethnicity. The gender and age group split reflects national findings. There was one record of a service user with a neuro developmental disorder – Autism, this person died due to an illicit drug overdose, intent unknown.
The deaths occurred across the trust with no apparent hotspots to date. The largest Care Groups within the trust with the highest population are North Norfolk and City and East Suffolk therefore numbers in these areas are expected to be higher. Equally both North Norfolk and East Suffolk have high levels of deprivation plus a mixture of rural and coastal villages and towns, these factors are known indicators for higher levels of neglect, self-neglect, drugs and alcohol misuse, suicide, and lower healthy life expectancy. The West and South Norfolk Care Group also have a high level of deprivation towards the West of the county and a low healthy life expectancy as well as an increasingly ageing population. The higher level of deaths in secure services relate in the main to people seen by the liaison and diversion teams based in police headquarters (21 out of 25 people). These people are invariably complex, the team is commissioned to undertake a primary assessment and offer signposting or recommendations for further assessment pre police interview, it is not a team that provides care and treatment.
Most people were open to a community team at the time of their death no-one was on a waiting list for assessment or post assessment in this cohort:
-
Findings and action
The trust has utilised the findings from all incidents of harm to service users to agree the patient safety incident priorities for 2023/24, these can be found within the Patient Safety Incident Response Plan on the trust website. Specific actions are outlined below in response to individual reviews and thematic reviews. In respect of drug related deaths, the patient safety team and operational colleagues have raised with system colleagues the concern around the need for a shared care pathway, this is being taken forward by the Integrated Care Boards.
Systems actions:
-
Drug and Alcohol training event in December 2022.
-
Menopause awareness training available to all staff, plus a webinar was held with a nationally acclaimed expert Dr Louise Newson April 2022
-
Autism training for all staff
-
Care Process audit schedule
-
STORM training roll out (risk assessment specific to suicide and deliberate self-harm)
-
Updated policies; missed ‘not brought’, clinical harm reviews, record keeping, clinical risk assessment.
-
Implementation of Standard Operating Polices for community and crisis teams; standardized
-
Roll out of DIALOG+, Formulation and Safety Planning
-
Stepping Back Safely programme for carers. Human Factors actions:
-
Real stories learning events for practitioners, 7-minute briefings and patient safety alerts in real time.
-
Culture – the psychological safety workstream is part of the trusts overarching improvement plan.
-
Targeted training in contextual safeguarding and use of the safeguarding escalation routes
-
Record keeping on trial – provided by external legal company October 2022
6.0 Medical Examiner Offices have been running in the 5 acute hospitals that serve the population of the Trust. The change in requirement under the implementation of the Medical Examiner for NSFT will be for those patients who the Trust currently certifies the death i.e., inpatients who do not fall under the coronial remit. These patients’ deaths will be of natural causes, typically in receipt of
end-of life-care who predominately die within the older person’s wards.
The purpose of the Medical Examiners system is to:
-
Provide greater safeguards for the public by ensuring independent scrutiny of all non- coronial deaths.
-
Ensure the appropriate direction of deaths to the coroner.
-
Provide a better service for the bereaved and an opportunity for them to raise any concerns to a doctor not involved in the care of the deceased.
-
Improve the quality of death certification.
-
Improve the quality of mortality data.
Following April’s ministerial statement, the National Medical Examiner expects all relevant deaths to be scrutinised by medical examiners by April 2024. NSFT have worked closely with the lead medical examiners in Norfolk to ensure we are working in line with national guidance and expectations. The Norfolk Medical examiners are kindly facilitating the training for the trust senior clinicians affected by the process and once completed implementation of the new system will occur.
The trust will be representatives on the Suffolk and North East Essex ICB Learning from Deaths programme including the implementation of the Medical Examiners implementation when introduced.
NSFT are actively represented at the Norfolk and Waveney ICB Learning from Deaths Forum which aims to share learning across the system. NSFT will ensure representation when a similar forum is developed by Suffolk and North East Essex ICB.
7.0 Grant Thornton UK LLP was commissioned by Norfolk and Waveney and Suffolk and North East Essex Integrated Care Boards and Norfolk and Suffolk NHS Foundation Trust to undertake a review of the systems and processes in place at the Norfolk and Suffolk NHS Foundation Trust (NSFT) for collecting, processing, and reporting on data relating to patient deaths. The review was performed in the period October 2022 to January 2023 and included data reporting and recording between April 2019 and October 2022.
The final report was published in June 2023 and an action plan has been developed with the agreement of the ICBs incorporating the improvements recommended for the Mortality process. Progress of the action plan is overseen by an Executive led Programme Management Board.
-
Conclusion and Next Steps
There has been significant investment by NSFT to enable access to data to provide information both strategically and locally to teams which will guide on where improvements need to focus. The Mortality action plans includes methods to enable closer working between the Patient Safety Team
/Mortality team and clinical services by facilitating learning sessions, sharing learning, and becoming
members/ attendees in local governance meetings. There are actions in place to enhance the Structured Judgement review process.
NSFT have an agreed process and system to refer all non-coronial deaths to the Medical Examiner system where the Trust are responsible for death certification, i.e., person in receipt of end-of-life care admitted to an Older Person’s ward. The Norfolk Medical Examiners are facilitating training for senior NSFT clinical staff on the purpose and expectations of the new statutory requirements. The newly developed process has been included in the Learning from Deaths policy.
-
Quality implications
New themes emerging from Mortality Reviews are incorporated into a programme of quality improvement. This will ensure we strive to reduce the health inequalities and improve the physical health care experienced by people with severe and enduring mental illness or a learning disability.
-
Impact on people who use services and their carers
Actions taken to address reversible causes of mortality, or the factors leading to them, will increase confidence in those who use our services and will reduce the harm from loss of loved ones.
-
Equality implications
The mortality process as noted is being reviewed and including the additional responsibilities of working with the medical examiners. The need for a case selection criteria process has been developed to ensure the focus is on people who experience health inequalities. This includes peoples living circumstances (deprivation), use of high dose medication in psychosis and those who experienced severe mental illness or a learning disability.
-
Financial implications
Recruitment for a dedicated Mortality Team Business Support/ Data Analyst and a Band 7 Investigation and Improvement Manager has been completed and team have been in place September 2023. The Interim Mortality Lead has been in place since January 2023.
-
Risks and mitigations
People who experience severe and enduring mental illness or a learning disability die 15-20 years sooner than other citizens. This is referred to as the mortality gap. Learning from Deaths aims to tackle these health inequalities. There is a risk that the data published is used or interpreted without context as there is no current national benchmarking or methodology within mental health and learning disability services for mortality.
Safeguarding
Annual Report
2022 - 2023
Trust safeguarding overview
Background:
Norfolk and Suffolk has a combined population of approx. 1,600,00 people. Two local safeguarding partnerships, two local authority counties, and two Integrated Care Boards.
The Trust has 11 Care Groups spanning all ages including specialist services; Secure (adults), Mother and Baby Unit
,Tier 4 Adolescent Unit, Learning Disability community and inpatient settings with approx. 4000 staff across all roles.
Trust safeguarding overview
• • •
Chief Nursing
-
Officer •
r t:kj
Norfolk and Suffolk
NHS Foundation Trust
J., NSFT CORPORATE SAFEGUARDING & PATIENT SAFETY
-
• •
Deputy Chief Nurse
Director for Nursing Suffolk & Workforce
CAIST Team Emilv Palmer (1 0)
Named Safeguarding Nurse
Associate Director of Quality Standards
Suffolk Care Groups Ser1Ior Leadership
l
Safeguarding Team
Clinical Safety Specialist (1.0)
Patient Safety Team Lead (1.0)
7x Safeguarding Specialist Practitioners
(0.4)-Aligned to West & South Norfolk Care Group (1.0)- Aligned to Norfolk CFYP and Specialist Services Care Groups
(1.0)- Aligned to Suffolk CFYP & West Suffolk Care
Groups
-
(1.0) Maternity leave-currently vacant- -Aligned to East Suffolk&, LD & Autism Care Groups
Vacant post (1.0)- Aligned to City & N. Norfolk, Wellbeing - Suffolk & Norfolk, Care Groups
-
Mat Cover {0.6)--Aligned to East Suffolk Care Group
-
(1.0) -Aligned to GY & Waveney, Secure and Forensic Care Groups
Bereavement & Suicide Prevention Advisor



(LO) Safeguarding Trainer and Communicatior1s Lead Vacant post- (1.0) DA Practitioner
(1.0) Admirli5trator
Trust safeguarding overview
-
Named Doctor for safeguarding children –vacant as of Summer 2021
-
An Expression of Interest is in progress
-
In the interim, the previous Named Dr for the Trust is jointly running the medic-specific safeguarding level 3 training.
-
Currently any concerns about safeguarding are discussed with the Trust Safeguarding Team.
-
If unable to recruit, discussions in progress to consider accessing resource from the Named GP/Doctors for Safeguarding within the ICS.
-
-
Safeguarding (154) and domestic abuse (67) champions across the Trust services.
-
The corporate safeguarding team provides; Safeguarding advice and support, the voice of Safeguarding in Care Group leadership and Governance Forums, Safeguarding training, complex case Safeguarding expertise at a team level , safeguarding supervision, Safeguarding awareness campaigns and briefings.
-
The team also screens complaints and incidents for Safeguarding concerns, undertakes professional and clinical incident reviews.
Trust Safeguarding Overview
|
Norfolk Safeguarding Boards |
Suffolk Safeguarding Partnership |
Community Safety Partnerships Suffolk and Norfolk |
General Safeguarding Forums |
|---|---|---|---|
Safeguarding Board Meetings | Safeguarding Board Meetings/Health Executive meeting | Domestic Abuse and Sexual Violence Steering Group Norfolk | Channel Panels Norfolk/Suffolk |
Health/Training Subgroups Children and Adults | Health/Training Subgroups Children and Adults | Violence Against Women and Girls Steering Group Suffolk | Domestic Abuse Health Forums- Suffolk/Norfolk |
Business Group | Learning and Improvement Groups Child and Adults | Local Community Safety Forums | MARACs |
Serious Adult Review Group | Safeguarding Adults Reviews | DHR Panels | MACE Meetings Suffolk/Norfolk |
Child Safeguarding Practice Review Panel | Child Case Review Group | MAPPA- Norfolk/Suffolk | |
LADO/SADS/Position of Trust |
The Safeguarding Team attend multiple external partner led safeguarding forums. Above are examples of some of these groups.
Contents:
-
Statutory duties
-
Governance
-
DATIX Safeguarding Reporting
-
Referrals overview and data
-
Safeguarding Consultation Audit 2022
-
Domestic Homicides, Safeguarding Adult Reviews, Child Safeguarding Practice Reviews, Mental Health Homicides
-
Training overview and data
-
Progress against 2022 – 2023 priorities
-
Priorities for 2023 – 2024 and linked workstreams
Legal framework and statutory duties
-
Children Act 1989/2018
-
Care Act 2014
-
Health and Social Care Act 2008/2012
-
Mental Health Act 1983/2007
-
Mental Capacity Act 2005
-
Deprivation of liberty safeguards - Liberty Protection Safeguards – due for implementation in April 2022/23 remain delayed until post term of current Government
-
Domestic Abuse Act 2020
-
Use of Force Act 2018
-
Counter Terrorism Act 2008
-
NHSE/I Safeguarding Policy
-
NSFT local policy and joint agency protocols
-
Local commissioners
-
Local Safeguarding and Community Safety Partnerships and Boards.

 Trust
Safeguarding Governance
Trust
Safeguarding Governance
Safeguarding Incidents/Concerns reported on DATIX
Safeguarding incidents reported on DATIX April 2022 to March 2023
250
200
150
100
50
0
Apr-22 May-22 Jun-22 Jul-22 Aug-22 Sep-22 Oct-22 Nov-22 Dec-22 Jan-23 Feb-23 Mar-23
Suffolk Norfolk
DATIX Reporting of Safeguarding Incidents/Referrals
-
The Safeguarding Policies direct best practice is for all safeguarding incidents and safeguarding referrals made, to be reported on Datix. This ensures the Safeguarding Team can maintain good oversight and provide additional safeguarding expertise and support for these patients, staff and teams.
-
2022/2023, the Team received on average 300 x safeguarding Datix per month, of which approximately 40% required a safeguarding referral for a child or adult at risk.
Safeguarding DATIX Key Themes:
-
Service User on Service User Assaults
-
Service User Assaults on staff
-
Sexual assaults/abuse disclosures
-
Domestic Abuse disclosures
-
Self Neglect
-
Neglect
-
Falls
-
The Safeguarding team were engaged in 2 x concerns escalated by NSFT practitioners of Modern Slavery
-
Norfolk- 3 x PREVENT Referrals and Suffolk- 0 x PREVENT Referrals
Referrals overview and data
NSFT Safeguarding Referrals Made April 2022 - March 2023
200
180
160
140
120
100
80
60
40
20
0
Q1 2022-2023 Q2 2022-2023 Q3 2022-2023 Q4 2022-2023
Norfolk Adult Suffolk Adult Norfolk Child Suffolk Child
Safeguarding Referrals- Adults
Safeguarding Adult Referrals Made April 2022 to March 2023
220
575
Suffolk adult referrals April 22-March 23 Norfolk adult referrals April 22-March 23
-
Suffolk ACS expectations of incidents that require referring to MASH are part of partnership agree Framework/ thresholds that require provider organisations to internally address small safeguarding issues proactively without referring for additional safeguarding specialist expertise.
-
Norfolk ACS expectations are that all incidents with any potential small s safeguarding concerns must all be referred to MASH. ACS social workers began to meet regularly with Acute and Older Person Services in Gt. Yarmouth and Waveney during this year, which is seen in the significant increase in safeguarding referrals and Datix reporting, made in Norfolk during quarter 4 this year.
Safeguarding Referrals- Children
Safeguarding Children Referrals Made April 2022 to March 2023
237
384
Norfolk children referrals April 22 to March 23 Suffolk Children referrals April 22 to March 23
Norfolk receive all child concerns through telephone consultation where social care will make the decision to refer/not refer as a safeguarding referral.
Suffolk expectation is for child safeguarding concerns to be escalated through the MASH portal as a safeguarding referral.
Safeguarding Referrals - Adults Categories
Suffolk Adult Safeguarding Concerns Referrals from NSFT – Abuse Categories
Sexual Negect Domestic Abuse Physical
Referrals overview and data
Norfolk Safeguarding Adult Concerns Referrals from NSFT- Concerns/Abuse Categories
SU to SU physical Physical Falls SU to SU Verbal Sexual Neglect
Referrals overview and data child safeguarding themes in referrals Norfolk and Suffolk
Suffolk Safeguarding Children Referral Categories April 2022-March 2023
Neglect Emotional Physical Sexual Self-harm Exploitation Domesitc Abuse Coercion
Referrals overview and data child safeguarding themes in referrals Norfolk and Suffolk
Norfolk Safeguarding Children referral Categories April 2022-March 2023
Neglect Emotional Physical Sexual Self-harm Exploitation Domesitc Abuse Coercion
Referrals overview and data
12
10
8
6
4
2
0
Apr-22 May-22 Jun-22 Jul-22 Aug-22 Sep-22 Oct-22 Nov-22 Dec-22 Jan-23 Feb-23 Mar-23
Suffolk Sec 42 - NSFT Suffolk Sec 42 - Police/ACS Suffolk Sec 42 ACS Norfolk Sec 42
Enquiry outcomes and learning are managed within localised teams with oversight from Care Group Governance Forums. In quarter 3, 2022/23 the Safeguarding Committee reviewed its Terms of Reference and governance to include expectation that each Care Group will report quarterly on this work to provide assurances on learning from these enquiries.
Referrals overview and data
Allegations Against Staff April 2022 - March 2023
9
8
7
6
5
4
3
2
1
0
Apr-22 May-22 Jun-22 Jul-22 Aug-22 Sep-22 Oct-22 Nov-22 Dec-22 Jan-23 Feb-23 Mar-23
Total NSFT Agency Unknown
The Safeguarding Team provide guidance and support to HR in identifying staff allegations where there are additional safeguarding concerns that will require LADO and/or Positions of Trust referrals. LADO and POT are multi agency forums led by ACS and Police that consider their additional internal intelligence that may contribute to supporting the Trust in recognising and managing additional safeguarding risks.
Referrals overview and data
LADO and Positions Of Trust Referrals made by NSFT April 2022 to March 2023
6
5
4
3
2
1
0
LADO - NSFT LADO - Agency POTS - NSFT POTS Agency
Norfolk Suffolk
Safeguarding Team Consultation Audit Findings
Safeguarding Inbox Audit - September to December 2022
On average the Safeguarding Team receive 1800 queries x per month. (average of 80 x per day )
-
27 queries x per day provide insufficient information
-
36 queries x per day do not require safeguarding specialist guidance and have not sought any line manager safeguarding guidance
-
10 queries x per day are queries about accessing training on ESR
-
25 queries x per week are complaints and not safeguarding issues
-
5 queries x per week are information only to seek reassurance rather than seeking Line Manager guidance, or are personal requests for guidance
-
On average, 10 x consultations per day are in relation to complex safeguarding concerns of abuse requiring additional guidance for safeguarding referrals and safeguarding expertise interventions.
Capital S - Concerns of significant abuse Safeguarding requiring safeguarding expertise and guidance are less than 15% of queries received.
Small S - safeguarding requiring proactive localised actions within individual risk assessments and care planning are more than 70% of queries received.
Safeguarding Team Consultation Audit Findings
The audit highlighted the Care Group areas where understanding of safeguarding and the confidence of practitioners in responding to local early safeguarding issues requires additional safeguarding workshops and training to take place, 2023/2024. Further work with Safeguarding Champions is planned to facilitate sharing of further resources that will support staff safeguarding decision making. The Team plan to review and improve safeguarding supervision availability for all staff for 2023/2024.
Safeguarding consultations where issues not requiring Specialist Safeguarding advice
Safeguarding consultations where issues not related to safeguarding
Great Yarmouth Acute Norfolk CFYP
Wellbeing Suffolk Wellbeing Norfolk
West Suffolk MHLT West Norfolk CMHT Central and North Older Persons CMHT Central and North CRHT East Suffolk Central IDT
Wellbeing Suffolk Norfolk CFYP
Central and North CMHT
Domestic Homicides and NHSE mental health homicide reviews
In 2021-22 the trust continued to be involved in six domestic homicide reviews from 2021/2022, and an additional DHR commissioned late 2022, where progression had been delayed due to Court hearings and DHR commenced early 2023. The Trust engagement in DHRs provides analysis of mental health care and treatment where either the perpetrator, victim, or both were/are known to the trust.
-
Perpetrator AS known to the liaison and diversion team. Gorleston, Waveney.
-
Perpetrator CC known to central Norfolk Early Intervention Team. Norwich.
-
Perpetrator RF known to crisis team central Norfolk. Shipdham.
-
Victim CW known to Norfolk assessment team in 2019. Suicide. CW died in Cheshire.
-
Victim and perpetrator known NM, CMHT open, and LM seen by mental health liaison service.
West Norfolk
-
Perpetrator PKB known to CMHT discharged in March 2021, offence June 2020. Gorleston, Waveney.
-
One of the victims, LN, open to CAMHS, Suffolk.
Child Safeguarding Practice Review; two published in this period.
-
Norfolk Child Safeguarding Practice Review. Published December 2022 - AL
Norfolk Safeguarding Children Partnership commissioned this Child Safeguarding Practice Review (CSPR)1 to learn from the circumstances of AL’s death. At the Rapid Review shortly after AL’s death the complex inter-play between mental health, for either a child or a parent, and safeguarding children was noted as a key area for this CSPR to consider
-
Norfolk Child Safeguarding Practice Review. Published January 2023 - AK
Norfolk Children Partnership were notified of the sad death of Child AK. At the point of referral, it was suspected that Child AK died as a result of overlay whilst in her mother’s care; mother was allegedly under the influence of drugs and alcohol at the time.
Child Safeguarding Practice Review; two published in this period.
Key Trust Learning From AL and AK CSPRs:
-
Improving working with fathers and father figures: The Lead Nurse for MBU and Perinatal Services and CAIST Safeguarding Specialist are engaged in the Safeguarding Partnership workstream to moving forward with this work across the Norfolk ICS. New assessment templates and approaches have been adopted within the Trust to ensure fathers and father figures are integral to assessments and care planning.
-
Disguised compliance: The Trust is reviewing the ‘Was Not Brought ‘ Policy and regular communications are shared through Patient Safety Newsletters and briefings to ensure this is a high consideration when working with children where there are concerns relating to engagement in their assessment , care and treatment.
-
The need to consider the whole family within child assessments, risk management, care planning and treatment. ‘Think Family’: The Safeguarding Team are leading on a Quality Improvement Project to improve Trust systems and processes that will support practitioners in recognising and understanding family and significant others needs alongside those of the child, to better inform robust risk assessing and care planning. This work is progressing 2023/2024, to ensure this work is aligned to the Trust plans to improve Electronic Patient Records systems and the use of electronic Genograms.
Internal Safeguarding Actions
Internal Patient Safety Reviews and a Safeguarding led audit into safety in discharge planning has led to key learning and actions to improve recognising and responding to safeguarding across the Trust:
-
Improving accessibility of level 3 safeguarding training
-
Provision of Domestic Abuse training on completing DASH Assessments
-
Access to safeguarding supervision for all staff
-
Improving oversight of internal statutory safeguarding enquiries and the learning.
-
Developing tools to support staff in completing DATIX for safeguarding incidents.
-
Improving safeguarding communications trust wide
Training
-
Late Summer 2022, the Safeguarding (SG) Team commissioned an additional safeguarding trainer role to deliver training and update all level 3 and bespoke safeguarding training packages.
-
The Trust have been working towards achieving improved compliance with safeguarding training across the Trust. This year the Safeguarding Trainer has been working on a safeguarding training plan that aims to achieve and maintain a higher level of safeguarding competencies across the Trust, of 90% and above from 2023/2024.
-
Safeguarding awareness is now integral to new staff Induction training.
|
Title |
Delivery |
% 11.07.22 |
% 27.03.23 |
±% diff |
|---|---|---|---|---|
Adults L1 | e-learning | 86.6 | 93.6 | +7 |
Adults L3 | SG Team | 79.9 | 84.7 | +4.8 |
Child L1 | e-learning | 84.6 | 88.6 | +4 |
Child L2 | e-learning | 83.6 | 91.8 | +8.2 |
Child L3 | SG Team | 83.9 | 81.7 | -2.2 |
Training
Regular Feedback from Safeguarding Training is now sought to further improve and tailor training workshops to the competency needs of staff, and to encourage reflection on sessions that formulates how the training will influence and impact on an individual’s professional practice.
A full day workshop is too intense
Training delivery is excellent and inclusive
A new Workbook approach is to be introduced May 2023 to support bitesize training opportunities. This approach will mandate individual reflection on safeguarding practice and how learning from training will impact in their clinical work.
Virtual training is difficult when so intense and prefer face to face workshops
Excellent training – Interactive and covers so much information on safeguarding
Need bitesize training on specific areas of safeguarding relevant to my practice
Training
Training Priorities for 2023/2024
-
To move to annual level 3 safeguarding training requirements within a Workbook approach- monthly audits of Workbooks will take place to monitor quality of training accessed and embedding of learning in practice.
-
To audit staff safeguarding skills and competencies Autumn 2023, to better understand training needs 2024.
-
To improve compliance with safeguarding training through providing sessions for Medics in protected training days, bespoke training for pharmacy staff and access to safeguarding training for Band 8s.
-
Link Safeguarding with Patient Safety and Clinical Safety Induction Training.
-
Continue to seek staff feedback on training.
-
Move to including persons by experience in aspects of safeguarding training provision.
2022/23 Safeguarding priorities/Updates
-
There has been a national rise in domestic abuse and homicides; this is reflected in our advice calls, training requests and Norfolk data - This year has seen bespoke training on completing DASH assessments for high risk Domestic Abuse across many of our services. A new system to gather information from relevant teams, and inclusive of safeguarding specialist practitioners attendance at all MARACs (high risk Domestic Abuse Multi Agency case discussions), safeguarding specialist attendance in ICS Domestic Abuse Health and Police led strategic forums, ensures the Trust is a partner agency in tackling Domestic Abuse across Norfolk and Suffolk.
-
There have been two sexual assaults in the trust; due to the pandemic the QI project stalled, however this must be a priority. The Sexual Safety QI Project is to recommence 2023. The Safeguarding Team are recruiting a Specialist Domestic Abuse Practitioner role
, summer 2023. 2022/2023 Patient Safety weekly huddles were in place to monitor incident reporting of assaults and escalating of safeguarding referrals and enquiries. Safeguarding specialist advice and support is provided for these cases. HR work closely with the safeguarding team in managing allegations of sexual assaults by staff.
-
The consistent theme in allegations made against staff is boundaries; relational security was part of a themed review within secure services in 2021. This is also a theme within our NMC referrals over 2020/21. HR and safeguarding work closely in managing allegations against staff where there are additional safeguarding concerns. They participate in relevant LADO and Positions of Trust Forums. Allegations against staff investigations are to be managed completely through HR and local Care Group processes with guidance from safeguarding to ensure proportionate sharing and storage of personal staff information. New systems and database are being established 2023/2024, to ensure data is provided to enable evidencing of safety of staff and patients in Safeguarding Assurance Reporting.
2023/24 Safeguarding priorities
-
To improve and maintain level 3 safeguarding training above 90% compliance.
-
To complete regular audits to improve and evidence quality in impact of training in practice.
-
To move to persons by experience participating in Trust safeguarding training sessions.
-
To improve advice and guidance on Domestic Abuse for staff and patients through improved training for DA Champions and recruiting of a DA Practitioner.
-
To provide Safeguarding Workshops that will build on confidence and competencies of staff in responding to local potential safeguarding concerns and risks within individual risk assessing and care planning and ensuring Safeguarding of significant potential or real harm from abuse, is escalated through safeguarding referrals.
-
To review and revisit QI Project for sexual safety.
-
To improve accessibility to safeguarding supervision for all staff trust wide.
-
To continue to improve safeguarding working relationships with external partner organisations.
-
To progress a QI Think Family project alongside the new EPR system work.
-
To continue to improve engagement of fathers and father figures in working with children and young people.
-
To be fully engaged and proactive in Safeguarding Partnership and ICS Safeguarding workstreams.
Additional workstreams which support safeguarding
-
Use of Force Act and reduction of restrictive interventions; co-produced literature for patients, enhanced demographic monitoring, review of policy, refresh of PMA training- Restrictive Interventions Lead.
-
Improving access to mental health; addressing mental health inequalities national QI project. Recruitment of an Equality and Diversity Inequalities Practitioner, patient facing, to the customer service team.
-
Review and publication of our Trust Suicide Prevention Strategy is to take place Autumn 2023. This strategy is aligned to the development of both counties’ Public Health, and the National Suicide Prevention Strategies.
-
Patient Safety Trust key priorities for 2023/2024 are influenced by key safeguarding themes, trends and information, and are developed in collaboration with safeguarding, complaints, PPL, quality and patient safety leads.

nsft.nhs.uk @NSFTtweets NSFTrust
|
Report to: |
Board of Directors |
|---|---|
Meeting date: | 23rd November 2023 |
Title of report: | Annual Director of Infection Prevention & Control (IPC) Report 2022/23 |
Purpose of paper: | For information and assurance |
Author: | Elaine Thrower, Lead Infection Prevention & Control Nurse and Deputy Director Infection Prevention & Control Natalie Wilkin, Infection Prevention & Control Nurse Specialist |
Director: | Tumi Banda, Interim Chief Nurse |
How this paper impacts on Trust Strategic Objectives | Exceptional care |
Legislation/Compliance |
|
How this paper impacts on current risks in Corporate Risk Register or BAF | BAF risk 2.1 risk of failure to deliver high standards of quality safety and effectiveness IPC Board Assurance Framework |
Executive summary
The purpose of this report is to inform the Board of the infection prevention and control work undertaken and provide assurance that the Director Infection Prevention & Control (DIPC) and Infection Prevention & Control Committee are discharging their accountability.
This report collates and summarises information related to healthcare acquired infection for the period 1st April 2022 to 31st March 2023. It also shows the progress made against delivery of the infection prevention and control annual programme and describes the management structure and oversight approach to prevention of infection in NSFT.
COVID-19 and other infections such as Norovirus and Influenza continued to challenge during 2022-
23. The DIPC and IPC team have been integral to support prevention and management of cases/ outbreaks alongside colleagues across the Trust to reduce the impact on service users and services. Throughout 2022-23, guidance on managing COVID-19 has evolved as the NHS implemented Living with COVID-19 . This has seen changes in admission screening, staff testing, mask use and care of those with Covid-19 infection.
Despite the demands on the IPC team, the majority of the IPC annual plan for 2022-23 has been met. Where actions were unable to be met, this was mitigated through risk assessment and prioritisation of actions to limit the impact.
Compliance with IPC standards has continued to be monitored through the IPC committee quarterly and a summary of actions, compliance and concerns is escalated to NSFT’s Quality Committee.
Recommendation
The Board is asked to review and approve the contents of this report for publication on the NSFT website.
Table of Contents
|
Item |
Description of item |
Page no |
|---|---|---|
1.0 | 2 | |
2.0 | 3 | |
3.0 | 4 | |
4.0 | 4 | |
5.0 | 5 | |
6.0 | 10 | |
7.0 | 14 | |
8.0 | 15 | |
8.0 | 15 | |
9.0 | 16 | |
10.0 | 17 | |
11.0 | 18 | |
12.0 | 18 | |
13.0 | 20 | |
14.0 | 22 |
Annual Director of Infection Prevention & Control (IPC) Report 2022/23
-
Introduction/Background
.1. The Trust recognises that the effective prevention and control of healthcare associated infections (HCAI’s) is essential to ensure that patients using our services receive safe and effective care.
.2. This annual report covers the reporting period of 1st April 2022 – 31st March 2023 and has been written in line with the 10 criteria outlined in the Health and Social Care Act 2008: Code of Practice in the Prevention and Control of Infection (updated December 2022) – see appendix 2 for details. The 10 criteria outlined in the code are used by the Care Quality Commission (CQC) to judge a registered provider on how it complies with legislation.
.3. In appendix 1 there is a list of abbreviations to aid the reader.
-
Key Achievements in 2022/23
-
There have been zero cases of MRSA bacteraemia, MSSA bacteraemia, and Gram-negative Bacteraemia notified to IPC team in NSFT during 2022-23.
-
The IPC Team participated in Patient-Led Assessments of the Care Environment (PLACE) during Autumn 2022 and NSFT achieved an overall score of 98.9% for cleanliness, (national average 98.01%).
-
The IPC team led on in-patient COVID-19 booster vaccination programme with 66 eligible in-patients were vaccinated during the Spring 2022 vaccine booster campaign and 110 eligible in-patients during Autumn 2022 vaccine booster campaign.
-
The IPC Team developed a Trust IPC Manual to incorporate standards as set in the NHS England’s National infection prevention and control manual for England and how these standards are practically applied within NSFT.
-
In relation to IPC team development, one team member was successfully awarded a master’s degree (MSc) qualification in Infection Prevention and Control after 3 years of part-time study.
-
During 2022/23, the IPC team have successfully secured funding and employed a substantive 1.0WTE Fit tester to continue to support staff resilience for respiratory protection.
-
The IPC team continued to carry out a large part of its audit programme despite ongoing demands of the COVID-19 pandemic and other clinical demands, this included: mattress checks, cleanliness, personal protective equipment use, hand hygiene checks, and quality ward walks and community site visits.
-
An Antimicrobial Lead is in place – appointed to a senior pharmacist in NSFT to support and champion good antimicrobial practice to reduce antimicrobial resistance as per the Department of Health and Social Care’s 5 year action plan: Tackling antimicrobial resistance 2019- 2024: The UK’s 5-year national action plan.
-
The IPC link nurse network has been successfully maintained, and support provided by the IPC team through network meetings and newsletters.
-
Reduction in contaminated needlestick injuries compared to previous 4-year average.
-
During the Autumn/ Winter period, a total of 68 clinics were provided to support staff to be vaccinated for Influenza and/or COVID-19. A 100% offer to all staff was achieved through an electronic vaccination system. Whilst uptake of the Influenza vaccine was lower than NSFT’s previous year’s uptake, 53.7% of frontline staff received their vaccine which was on par with the national average. 61.8% of frontline staff received their COVID-19 booster vaccination.
-
Challenges faced in 2022/23
-
Throughout 2022/23, infection case rates in NSFT have been higher than the pre-pandemic average. There continued to be considerable demand on the IPC team for managing and supporting cases and outbreaks of infection. Whilst COVID-19 case rates reduced compared to previous years, NSFT saw an increase in other infections (particularly Norovirus during Winter 2022/23).
-
There were challenges faced by the IPC team during quarter 3 (October - December) with completing some of the actions set in the IPC Annual Programme 2022/23. This was due to a vacant band 6 IPC nurse position for 3 months (August – November 2022) and the
delivery of the staff and in-patient vaccination campaign. This was mitigated through risk assessment by ensuring actions were prioritised and the IPC team were supported with additional staff resource to support the vaccination campaign.
-
During 2022/23, clinical staff compliance was 84% with IPC mandatory training.
-
Care Group representation at the IPC committee has been inconsistent throughout 2022/23 which impacts clinical involvement and the committee’s ability to discharge its responsibilities.
-
IPC Focus for 2023/24
-
Continue to provide clinical advice and specialist support to manage infection cases or outbreaks in NSFT
-
Continue to ensure written IPC guidance is evidence-based and kept up to date. Also ensuring IPC resources available on the intranet are appropriate and reviewed as required.
-
Continue to monitor compliance with IPC standards to minimise infection risks.
-
Re-introduction of IPC nurse visits to assess community clinic areas.
-
Implementation of an electronic audit system to provide greater oversight of IPC compliance.
-
Strengthen staff’s IPC knowledge through development of increased support to LIPACS (link nurses), delivery of clinical staff mandatory training via virtual training with an IPC nurse as an alternative to e-learning, introduction of specific antimicrobial training to prescribers and clinical staff administering medications to reduce antibiotic resistance and improve IPC education at staff induction.
-
Strengthen in-patient information on IPC in collaboration with people participation leads and communication team by developing an in-patient leaflet to be provided on admission on how patients can reduce infection risks.
-
Continue to deliver vaccinations (Influenza and COVID-19) to staff and patients as per national recommendations.
-
Continue to provide specialist input into major building refurbishment work. In addition to providing clinical support to the NSFT Water Safety and Ventilation Groups to support NSFT to meet all national recommendations as per the Health Building Notes (HBNs) and Health Technical Memoranda’s (HTMs ).
-
Continue activity with face fit testing of clinical staff to correctly wear Respiratory Protective Equipment (e.g. FFP3 type masks), to support organizational resilience for the management of cases of airborne infection.
-
Criterion 1
-
IPC Management within NSFT
-
At NSFT the position of Director of Infection Prevention and Control (DIPC) is nominated to the Deputy Chief Nurse who has overall responsibility for the IPC Team, acts as chair for the IPC Committee ensuring the committee discharges its duties in line with the terms of reference and has
responsibility for the strategic co-ordination of infection prevention and control activities; ensuring adequate resources, systems and polices are in place.
The IPC team is managed by the Lead IPC nurse. The IPC Team resource and structure was reviewed during 2022-23 and the team structure is shown in appendix 3.
The team has had some changes in staffing during 2022-23 with a band 6 IPC nurse resigning for a mental health nurse position in the community. The IPC team have successfully recruited to the post in November 2022 and a permanent 1.0 WTE fit tester was employed to support ongoing staff resilience to be prepared for response to respiratory infections spread by the airborne route.
The IPC team are responsible for:
-
maintaining an IPC Duty Nurse service to provide clinical support on case/outbreak management and response to relevant incidents (needlestick injuries, body fluid exposures and COVID-19);
-
monitoring, investigating and the reporting of cases of infection;
-
the provision of IPC practice guidance;
-
ensuring the provision and correct use of personal protective equipment;
-
ensuring suitable staff education and training is available;
-
giving advice for the nursing management of cases of infection;
-
overseeing of a programme of audit and quality improvement to ensure key policies and practices are implemented appropriately;
-
responding to risks reported through the Trust’s robust incident reporting system which comprehends reporting adverse incidents such as infection risks including individual or multiple cases of infection occurring in staff, patients or visitors, occupational exposure to potential blood borne virus events, risks escalated related to poor practice, and adverse results for microbiological testing of water quality;
-
supporting actions related to risks escalated to the Trust Risk Register that relate to infection prevention & control; and
-
regular review of the NHS England Infection Prevention & Control Board Assurance Framework with escalation in gaps in compliance to the DIPC and IPC Committee.
NSFT has continued to contract an Infection Control Doctor via a service level agreement from Cambridge University Hospitals who provides additional expert support to the IPC team as required.
Succession planning and development of team members has continued, with one team member successfully awarded a master’s degree (MSc) qualification in IPC in Summer 2022 and one team member commenced an NHS Leadership course in October 2022. To support continuing professional development and for Trust learning, the IPC team has ensured a member from the team has attended national and regional conferences and educational events.
To support the IPC team service, the Trust operates a system of link infection control practitioners known as Local Infection Prevention and Control Supporters (LIPACS). The aim of the LIPACS network is to support monitoring of standards, promote good practice and act as a link between the clinical team they work within and the IPC team. The LIPACS network has been maintained over 2022-23, with each in-patient area having at least 1 nominated LIPACS. During 2022-23 the IPC
team provided 2 virtual education days, a quarterly newsletter and ongoing support to LIPACS to help them with this role.
-
IPC Committee Structures and Assurance Processes
The Trust Infection Prevention and Control Committee is held quarterly and is chaired by the DIPC. Membership includes senior representation from the Care Groups and relevant corporate support services. The Committee provides a forum for oversight and monitoring of IPC compliance with the Health & Social Care Act 2008 Code of Practice (2022) through the following workstreams:
-
Board Assurance Framework
-
Annual IPC Programme
-
Annual Audit Programme
-
IPC Policy/ Guidance ratification, implementation, and monitoring
-
Monitoring infection data
-
Sharing learning from national, regional, and local forums
-
Identifying IPC risks and escalation as required
Following each IPC committee, a Chair’s report is produced and shared with the Quality Committee to provide assurance and escalate risks for the Trust Board’s awareness. The committee structure is shown in appendix 4.
The IPC team are members of the following committees/ meetings to support and champion IPC throughout the Trust:
-
Health & Safety Committee (Bi-monthly)
-
Water Safety Group (Quarterly)
-
Water Safety Operational Group (Monthly)
-
Workplace Health & Wellbeing (Quarterly)
-
Contract performance for domestic services (Quarterly)
-
Medicine Optimisation Committee including antimicrobial stewardship (Quarterly)
-
Estates and Facilities meeting (Monthly)
-
Project team for Rivers Centre – Hellesdon Hospital new build wards (Monthly)
-
Medical Devices Group (Quarterly)
-
Resuscitation Standards Group (Quarterly)
-
Physical Health Nurse Forum (Bi-Monthly)
In addition, the IPC team attend meetings held by the Integrated Care System (ICS) for Norfolk and Suffolk to support local and regional IPC initiatives. These initiatives include workstreams to reduce unnecessary glove use and reduce specific infections such as those affecting the blood stream, urinary tract and gastric system. Participation in the meetings convened by the ICS IPC teams also enables promotion of shared learning and resources, it facilitates a network of experts to tackle new and ongoing public health infection concerns, and strategic issues such as the stewardship of antibiotics.
-
CQC – IPC Assessment
The CQC met with and interviewed the DIPC and Lead IPC Nurse in November 2022. The CQC report published in February 2023 with positive feedback received for areas inspected, highlighting
staff were noted to be following infection control policy and clinical areas were clean. The report identified a minority of some clinical teams being below the CQC target of 75% compliance for mandatory infection control training. The IPC team will continue to provide support to clinical areas to improve compliance and monitor IPC training compliance through the IPC committee throughout 2023-24.
-
External reviews
The Trust was visited by the IPC nurse for Suffolk Integrated Care System (ICS) in July 2022. Three in-patient wards (Adult, Older People and Learning disability) in Ipswich were visited and positive feedback was received noting the environments and equipment were visible clean.
-
Patient-Led Assessments of the Care Environment (PLACE)
Following the cessation of PLACE inspections during the COVID-19 pandemic, these were re- introduced in 2022. The IPC team participated in PLACE inspections during Autumn 2022 to assist service users in their assessments of in-patient environments visited. NSFT’s was rated at 98.9% for cleanliness; 99.58% for food; 95.05% for privacy, dignity and wellbeing; 97.74% for condition appearance and maintenance; 96.93% for dementia; and 94.05% for disability. All scores were above the national average scores for 2022.
-
Infection Case/ Outbreak Surveillance and Management
The IPC Team provides clinical advice/ support via a telephone and email duty service Monday – Friday 9am - 5pm (excluding bank holidays). Out of Hours, support from the on-call manager and written IPC guidance is followed. Notification of an in-patient case of infection to the IPC team is through contact by the clinical team to a dedicated IPC duty email or by the clinical team completing a DATIX incident report.
Reportable Infections COVID-19
During 2022-23, the most significant infectious organism identified in NSFT continued to be the
COVID-19 virus (SARS-CoV-2). In total there has been 251 cases identified within NSFT inpatients, resulting in 42 outbreaks reported to NHS England and local Integrated Care Systems (ICS).
All confirmed cases identified are investigated to determine if they are associated with hospital stay as determined by applying the guidance set in the NHSEI CNO Letter (Ref No 001559) 19 May 2020.
|
Patients identified as Hospital onset COVID-19 infection |
|---|
Community-Onset (CO) - positive specimen date <=2 days after hospital admission or hospital attendance; |
Hospital-Onset Indeterminate Healthcare-Associated (HO.iHA) - positive specimen date 3-7 days after hospital admission;(this means that it is not possible to say whether the infection was acquired prior to hospital admission or after) |
Hospital-Onset Probable Healthcare-Associated (HO.pHA) – a positive specimen date 8-14 days after hospital admission;(this means that the infection was most probably acquired in hospital although community acquisition is also possible) |
Hospital-Onset Definite Healthcare-Associated (HO.dHA) – a positive specimen date 15 or more days after hospital admission; (this means that the infection was definitely acquired whilst a patient was in the hospital). |
Using the NHS England apportionment criteria, 80% of NSFT in-patient cases occurred in patients occupying a bed for 15 or more days. It should be noted that a proportion of those classed as Hospital
Onset Definite Healthcare Associated were patients who had utilised leave off NSFT wards (day leave, overnight leave, pre-discharge trials of leave) and it was not clear if acquisition of COVID-19 had occurred on the ward or during leave.
Of the 251 in-patient cases identified, 236 experienced mild symptoms or were asymptomatic. However sadly there were 14 cases who required additional treatment from a local acute hospital. Of these, 2 patients died within 28 days (One community acquired prior to admission and one definite hospital onset). A further patient died within 28 days of COVID-19 diagnosis (Indeterminate onset) within NSFT.
Please see appendix 5 for graphs showing NSFT COVID-19 case data during 2022-23.
The Trust has continually reviewed IPC guidance in relation to COVID-19 management during 2022- 23 in line with national guidance and evidence available. Trust communications has been utilised to share key messages with staff, patients, carers, and visitors.
Mandatory Surveillance Organisms
There have been zero cases of MRSA bacteraemia, MSSA bacteraemia, and Gram-negative Bacteraemia notified to IPC team in NSFT during 2022-23.
There has been 1 case of Clostridium Difficile infection detected during 2022-23. A post infection review was completed. The patient made a full recovery from this infection. The ward team applied appropriate infection control measures and no further cases were identified.
Notifiable Infections
During 2022-23, there was one case of notifiable infection identified in an NSFT in-patient with Salmonella infection which was community acquired (prior to hospital admission). Support was provided to UK Health Security Agency (UKHSA) by the ward clinical team and the IPC team on their investigation. The patient was provided appropriate care and treatment led by the patient’s medical team and local microbiologist. The ward team applied appropriate infection control measures and no further cases were identified.
Non-Reportable Infections Influenza
There was one Influenza outbreak identified during 2022-23 on an older people’s inpatient ward,
which identified 7 confirmed patient cases with Influenza A through laboratory specimens and 7 suspected staff cases with influenza-like-illness symptoms. 2 of the patient cases required additional treatment at the local acute hospital for their symptoms and returned to NSFT care following treatment. National guidance was followed to control the spread of infection and anti-viral treatment was utilised during this outbreak.
Other Respiratory Infections
During Autumn/Winter 2022-23 included one case of Rhinovirus (common cold) and one case co- infected with respiratory syncytial virus (RSV) & Human metapneumovirus (hMPV).
Norovirus
Norovirus (often known as winter vomiting virus) is a short lived, vomiting and diarrhoeal illness which is highly transmissible to other people. During Autumn/Winter 2022-23, NSFT identified 10 confirmed
in-patient cases and 36 possible in-patient cases of Norovirus resulting in 8 in-patient outbreaks. Predominantly areas affected were older people’s in-patient wards. There were 4 patients who were admitted to the local acute hospital for further treatment, and sadly one of these patients died shortly after diagnosis of being Norovirus positive.
Whilst this is higher than usual activity for NSFT, national surveillance data for Norovirus has shown a significant rise in Norovirus cases over the Autumn/Winter 22-23, compared with the pre-pandemic 5-year average (pre-pandemic average used as case rates significantly lower during the COVID-19 pandemic due to measures in place e.g., social distancing, isolation so not a true representation).
Please see appendix 6 for NSFT 2022/23 Norovirus data and national UKHSA data for Norovirus laboratory data in England by week during 2021 to 2022 and 2022 to 2023 seasons, compared to 5- year season average.
Skin & Soft Tissue Infections
There was 1 confirmed case identified of Group A Streptococcus infection from a wound identified in an in-patient during 2022-23 that was successfully treated with oral antibiotics. In addition, there was 1 in-patient case treated with oral antibiotics based on recent contact history with a suspected Group A Streptococcus case and who had relevant symptoms, but laboratory specimen was negative for bacterial causes.
There was 1 in-patient case of Methicillin-Resistant Staphylococcus aureus (MRSA) colonisation (carrier) identified in an in-patient with a previous history of MRSA. The patient received de- colonisation therapy to reduce the risk of developing a bacteraemia (bloodstream infection).
Other Infections
There was 1 in-patient (paediatric) case of Chickenpox identified during 2022-23. The case was classified as community acquired as known to have had contact with other cases prior to admission. The case resolved with no further complications and no further cases were identified on the ward.
Antibiotic Resistant Organisms
During 2022-23, 1 in-patient had been identified as positive for Carbapenemase-producing Enterobacteriaceae (CPE) carriage prior to admission to NSFT. CPE are gram negative bacteria which are resistant to carbapenem antibiotics, which can make treatment ineffective. The Trust has guidance on CPE which is available on the Trust intranet for staff to access and this was followed.
No patient cases of extended spectrum Beta-lactamase (ESBL) producing gram negative organisms were reported to the IPC team during 2022-23.
6.0 Criterion 2
-
Decontamination & Cleanliness
Oversight of decontamination is undertaken by the IPC Committee. Methods in Trust policy and process are in line with the national IPC manual and during 2022-23 the Trust fully implemented the updated National Standards of Healthcare Cleanliness 2021.
Domestic services across Trust buildings (with the exception of Wedgwood House), continues to be delivered by G4S. The change of service hours has been embedded with no new issues identified. Operational oversight of the contract performance continues by the Facilities management team.
The Wedgwood Unit at the West Suffolk Hospital site remains under supply provided by GFM.
Additional cleaning resource has also been utilised throughout 2022-23 to support rapid clinical cleaning and terminal cleaning following patient discharge and outbreak events.
The quality of the service provision is monitored by a structured and adhoc programme of audits conducted by the NSFT Facilities contract compliance team in accordance with the National Specification for Cleanliness. In line with the National Standards of Healthcare Cleanliness 2021, all Trust areas display a cleaning charter and cleaning scores to evidence compliance with the standards.
Areas of domestic cleaning failure are recorded for domestic supervisor and management rectification. The IPC team participate in quarterly contract performance monitoring of the G4S provision and continue to work closely with the contract compliance team and the contracted domestic services providers.
Medical/patient equipment cleaning continues to be the responsibility of clinical staff. Compliance with processes to ensure after-usage cleaning and the cleaning of infrequent use items is undertaken is checked by the IPC team on ward walk rounds/ site visits with feedback given to the team at each visit.
Throughout 2022-23, inpatient LIPACS (link IPC nurses) have completed an audit on patient equipment cleanliness as part of the annual IPC audit programme. Audit results are presented in appendix 7. Areas identified as needing improvement were fed back to ward teams, matrons, and lead nurses for action. In addition, the IPC team created a specific cleaning information pack for clinical staff which was shared and circulated to in-patient clinical staff through the Trust safety bulletin and IPC newsletter.
-
Laundry
The laundry provision has continued to be contracted to Elis Berendsen. Processes for the management of infected laundry have been managed in line with the Department of Health guidance HTM 01-04. There has been no supply issue or concerns raised during 2022-23.
-
Waste
The IPC team and Facilities management teams work in partnership to ensure compliance with National Health Technical Memoranda for management of hospital waste. This partnership includes assessment of safety with waste segregation, waste facilities cleanliness, security, and suitability. Processes for waste management are outlined in a Trust policy. Contracts for waste management and removal in Norfolk and Suffolk are in place. Waste streams in operation are infectious, domestic (including WEE waste), recycling, sharps, and medicinal waste. A Trust waste policy is in place and in alignment with the requirements of National guidance.
-
Water Safety
The IPC team continue to support the monitoring of water systems through membership of the Water Safety Group and also through the Water Safety Operational Group. The Water Safety Group met quarterly during 22-23. This is a strategic level assurance group which provides a formal report to
the Health & Safety Committee. Terms of Reference are in place with membership including external contracted Authorised Engineer [Water] services from Hydrop Ltd. A Water Safety Plan is in place which is overseen by external expertise from Hydrop Ltd.
Regular monitoring of water safety and quality is under the remit of the Water Safety Operational Group (WSOG) which meets monthly; twelve meetings were held in the year. It is through the WSOG members that the Water Safety Plan is operationalised. Members of the WSOG have undertaken specialist water safety training to meet the requirements of the water safety plan. It is through this group that the training of all staff who work on the water system or provide advice for clinical or system management is monitored. Training compliance has improved across the last year with 4 members of the IPC team undertaking City & Guilds accredited Legionella and water quality risk management - Responsible Persons training.
Working under the plan during 2022-2023 included the continued monitoring of water quality as part of risk management of Trust properties where system design or operational factors bring limitations to the control measures that can be deployed to prevent the growth of bacteria such as legionella. The WSOG with support from the Authoring Engineer (Hydrop Ltd.) have successfully managed remedial interventions where adverse results from microbiological testing have been identified. No patient has been reported as a case of hospital onset legionella infection.
The WSOG have supported a number of refurbishment projects where upgrade to sanitaryware was within the scheme. This work included Rollesby Ward, Wedgewood House 136 suite, Blickling Ward and Great Yarmouth Acute service. The WSOG promotes the use of sinks, taps and baths to have programmable sensors which purge water periodically to avoid stagnation. Capital investment will see the continued use of these automated water controls in wards and in community bases.
Of the new build projects water system designs have been reviewed and commissioning assurance achieved, this included Northside House - Drayton ward and the pharmacy in Woodpecker House. Ongoing work is expected with the Rivers Centre development at Hellesdon Hospital.
A key workstream for water safety activity has been centred on the response to an action plan from an audit of water safety governance which was undertaken by Hydrop Ltd. during August and September (see appendix 8). The overall assurance remained at reasonable, with areas for action including:-
-
implementing a process for contractor competency assurance;
-
improving governance for defect management for water system defects identified through expert led risk assessments of individual buildings and sites;
-
implementation of Zetasafe® (a software system for managing compliance with planned maintenance tasks on the water system, which enables dashboard oversight)
-
recommencing post pandemic, external support for water system risk assessment of Trust buildings by water safety experts;
-
assurance on flushing of infrequently used water outlets such as taps, showers, baths with full Trust mapping of buildings onto a flushing recording software system used by the Trust (L8 Guard);
-
continued work towards the availability of water system schematics for all Trust properties.
Of note during the year there has been the successful roll out of Zetasafe to the mobile phones of maintenance staff to enable improved data on pre-planned maintenance compliance. Whilst flushing compliance assurance continues as a concern, through regular monitoring using L8Guard recording software, and IPC team report to ward managers, an improving trend in consistency with completion of outlet usage assessment, (and the subsequent flushing of low use outlets), has been noted. Continued work to support clinical engagement with water safety by ward staff has initiated the development of a training session on MS Teams. Further work will be the roll out of heat maps created by the Estates to aid and direct flushing activity.
-
Ventilation
The Ventilation Safety Group (VSG) was established in response to the updated Health Technical Memorandum 03 – 01: Specialised ventilation for healthcare premises (Parts A and B) 2021 and to support compliance with the Infection Prevention & Control Code of Practice, and the national guidance from UKHSA which included ventilation as a key aspect of engineering controls for the management of infection within the hierarchy of controls framework. The monitoring and management of ventilation systems are also noted to be within the key lines of enquiry in National Infection Prevention & Control Board Assurance Framework (NHS England 2023).
The aim of the VSG is to monitor and advise on ventilation within Trust properties and buildings occupied by staff and patients. To work towards compliance with national documentation and to use the VSG as a forum for monitoring and overview of ventilation issues, risks, and to act as an assurance group for review of operational management of existing ventilation systems, and to give support to the design and commissioning of new systems.
The inaugural meeting of the VSG took place April 22. Terms of reference have been devised to ensure appropriate Trust representation. There has yet to be the successful appointment of a contracted service for Authorising Engineer [Ventilation]. The VSG met four times during the year. The VSG is a sub-group of the Health & Safety Committee.
Activity of the VSG included the oversight of the design and commissioning of ventilation systems in Wedgewood 136 suite and seclusion area, Drayton ward refurbishment and extension, Sandringham ward new air handling installation, Hellesdon refit gym, Rollesby ward and remedial work to the system in Hammerton Court wards.
-
IPC & the Built Environment (Estate)
The IPC team has completed environmental audits of all NSFT in-patient sites during 2022-23, with action plans and feedback provided to each ward team.
The IPC team alongside estates/maintenance colleagues have supported the following refurbishments:
-
Great Yarmouth Acute Services (Adult) – additional hand wash basin provision, upgrade to storage areas (clinical, food and linen), en-suite upgrades, clinic room upgrade, and shared bathroom upgrades. This work was expected to be completed during 2022-23, but due to clinical pressures and supply of materials/labour, it is expected to be completed summer 2023.
-
Blickling Ward (Older People) – the IPC team was consulted for the refurbishment of Blickling ward as part of the work to reduce ligatures.
-
Drayton Ward (Secure Services) – has undergone a large refurbishment project which saw the ward extended to enable all bedrooms to be en-suite and provide better clinical spaces for staff to suitably apply IPC measures. The project is expected to be completed in 2023.
-
Woodpecker House Pharmacy dispensary; a new build project
-
Refurbishment of Rollesby ward which included upgrade to existing sanitary ware.
-
Wedgewood House, refurbishment of the 136 Suite
In addition, the IPC team have consulted on the design of the new development at the Hellesdon Hospital site. Rivers Centre which will comprise of 3 new adult mental health wards and a hub area. The IPC team will continue to be involved throughout all building stages to ensure the Trust complies with HBN Infection Control & the Built Environment 00-09.
7.0 Criterion 3
The Trust has the following support in place to optimise patient outcomes and manage infection appropriately reducing the risk of adverse events and antimicrobial resistance.
-
The Trust has appointed a senior Pharmacist to direct antimicrobial stewardship within the organization.
-
The Medicines Optimisation Committee has oversight of antimicrobial use as part of medicines management, which includes approval of the NSFT stewardship guidance and publication of approved primacy care formularies which support prescribers in decision making on antimicrobial use, and also considers local microbiological sensitivity patterns of common bacterial infections.
-
The Trust has access to 3 acute hospital laboratories for microbiology support and infection diagnosis, with reporting on tests direct to clinical staff to aid management.
-

 The
Trust has access to a Consultant Microbiologist Infection Control
Doctor for complex case discussion via a contractual agreement
with UKHSA laboratory Addenbrookes Hospital.
The
Trust has access to a Consultant Microbiologist Infection Control
Doctor for complex case discussion via a contractual agreement
with UKHSA laboratory Addenbrookes Hospital. -
The Trust IPC team support the workstreams on healthcare associated infections including resistant organisms led by NHS Norfolk & Waveney and NHS Suffolk and Northeast Essex Integrated Care Boards. This work includes Clostridioides difficile, MRSA and Gram-negative infection focus, in addition to sharing and learning for more generic infection reduction strategies related to promotion of hydration as a urinary tract infection prevention tactic and reducing inappropriate use of Personal Protective Equipment, specifically glove use. See figure 2 below for an example of the glove use awareness in
NSFT which has been undertaken as part of this collective work. Figure 2
-

 During
the year IPC supported clinical teams to safely manage 1 case of a
patient colonised with Carbapenemase-producing Enterobacteriaceae
(CPE) and 1 patient for MRSA skin colonisation. 1 inpatient case
of Clostridioides
During
the year IPC supported clinical teams to safely manage 1 case of a
patient colonised with Carbapenemase-producing Enterobacteriaceae
(CPE) and 1 patient for MRSA skin colonisation. 1 inpatient case
of Clostridioides
difficile infection did not identify antibiotic prescribing as a concern in the post infection review.
-
Antibiotic awareness week (18th-24th November) was recognized in the Trust through communications
-
The IPC team continued to lead on ensuring inpatients who are unable to access seasonal vaccines are offered their influenza vaccine and COVID -19 booster.
-
66 inpatients received a spring booster for COVID-19
-
112 inpatients received an autumn booster for COVID-19
-
61 inpatients were prescribed a flu vaccine
-
-
Future work for NSFT will focus on 2 key workstreams
-
the garnering of data for antimicrobial prescribing and administration using the MEG electronic medicines management audit tool.
-
Promoting electronic learning resources for clinical staff who prescribe and/ or administer antimicrobial medications.
-
8.0 Criterion 4
The NSFT internet site includes information for patients, visitors, and the public on keeping you safe from infection and COVID-19.
Information includes:
-
How you can help us fight infection
-
Hand Hygiene
-
Help us fight flu by getting vaccinated
-
Statement of compliance
-
COVID-19 Information on visiting arrangements
-
COVID-19 Support for carers
-
COVID-19 Help keep our hospital safe
-
COVID-19 Our staff discuss the COVID-19 vaccination
-
Links to national COVID-19 Guidance
The IPC team has continued to provide expert advice on visiting to in-patient services. Development of information resources to support visiting and for patients who are asked to isolate from others due to an infection concern has commenced.
-
Criterion 5
-
Admission Infection Assessment
The electronic inpatient admission form for Physical Health facilitates the identification of infection issues including a prompt to check recent infection events. Compliance is monitored as part of the quality and safety reviews.
During 2022-23 there were changes to COVID-19 admission testing as per national guidance. Where national guidance recommended testing, this was achieved through point of care testing where available or lateral flow device tests at ward level. This enabled timely results to aid assessment of infection risks. In addition, PCR testing via local laboratory was also available as appropriate.
Vaccination status for COVID-19 and Influenza vaccines is checked as appropriate by ward-based pharmacist for newly admitted patients. This supports both risk assessment understanding the infection vulnerability of the person and offering vaccination within NSFT where available.
-
Infection Alerts
Within the electronic care record (Lorenzo) an alert can be created for infection risks to aid communication within the Trust. In addition, the Trust utilises the incident reporting system (DATIX) to document infection cases, and this automatically populates an email to relevant managers/ departments (including IPC Team) to alert them to a new infection case.
The IPC team are informed of infection cases through the following routes:
-
Directly from the clinical team
-
From communication with other IPC teams within the region
-
Direct from the Microbiologist/ local laboratory (usually following previous case discussion or result of significance)
-
Specialist IPC Advice
NSFT staff are able to gain specialist advice on the management and treatment of infection cases through the following routes:
-
IPC duty nurse (Mon – Fri 9am-5pm, exc. bank holidays)
-
IPC written guidance on the NSFT staff intranet site
-
National written guidance (gov.uk website, UKHSA website, NICE Guidance)
-
Discussion with local duty microbiologist (usually medical advice on treatment based on specimen results)
-
The IPC team are able to discuss cases with the Trust’s contracted Infection Control Doctor.
-
Criterion 6
-
Mandatory IPC Training
IPC education is a fundamental aspect to ensure staff have the knowledge of expected IPC standards. The Trust uses the national e-learning for healthcare infection control training package. Clinical staff are expected to complete level 2 e-learning annually and non-clinical staff to complete level 1 every 3 years. During 2022/23, compliance with mandatory IPC training was 84% for clinical staff and 92.5% for non-clinical staff. Whilst clinical staff did not meet the required 90% threshold, this is an improvement of 5.5% compliance. Training compliance is monitored quarterly by the IPC
team and presented to the IPC Committee. Compliance data is fed back at ward level and to care group lead nurses.
An aim of 2023/24 is to improve compliance of mandatory IPC training for clinical staff with the implementation of training being delivered by the IPC team via Microsoft teams. Whilst e-learning will still be available for staff to access, it is hoped that it will help staff who find e-learning challenging. Furthermore, the IPC team hopes to strengthen IPC training for new starters joining the Trust and will be working with the education induction team in how this can be delivered.
-
Link IPC Nurse (LIPACS) Training
The IPC team continued to provide support to newly appointed LIPACS at an individual level via visits to their area of work or via a virtual meeting to provide support. In 2023/24, the IPC Team aim to set up a formal programme of LIPACS training which will give them further enhanced IPC knowledge and skills to complete this role.
During 2022/23, the IPC team facilitated 2 remote network education half days using Microsoft teams and continued to produce a quarterly newsletter to help LIPACS, ward managers and matrons keep up to date with IPC changes. It is hoped in 2023/24 a face-to-face education day can be facilitated for LIPACS to support their increased knowledge, share learning and experiences and network with other LIPACS across the Trust.
-
Trust Wide Learning
The IPC team utilises Trust email communications and safety together bulletins to help keep staff informed of important changes or disseminate important learning following IPC related incidents. During 2022/23 the IPC team has used the Trust Safety Together Bulletin to communicate: how to prevent sharps injuries; water safety; cleaning refresher; winter vaccinations; winter illnesses (Influenza, Norovirus); FFP3 masks; and glove awareness.
-
IPC Team Development
During 2022/23, members of the IPC team have had the opportunity to undertake the following courses/ events to progress their learning:
-
One staff member successfully completed a Master’s level Infection Prevention & Control qualification
-
One staff member commenced an NHS Leadership Rosalind Franklin course with completion aimed in June 2023
-
One staff member attended the annual Infection Prevention Society conference – 3 days
-
IPS regional conference and network meetings were attended by one or more of the IPC team
-
Water Safety – one member achieved the 3-day Responsible Persons course and 2 members completed refresher training
-
Criterion 7
Patient assessment of physical health is expected at the point of admission. This assessment is used to aid placement and the need for isolation due to suspected or confirmed infection. During
outbreak incidents the isolation and cohorting of patients with symptoms or confirmed infection was prioritised. Use of risk assessment continued to manage available beds for admissions in settings where infection was present.
Challenges continued with the management of patients who for cognitive impairment or acute mental illness presentation were unable to isolate in their bedroom. Risk mitigation strategies were deployed to reduce the risk of transmission in inpatient settings. The inability to remain isolated when infectious likely contributed to outbreak of both respiratory and gastrointestinal illness.
Whilst the Trust in-patient environments consist of single accommodation rooms. Not all inpatient accommodation is able to offer an en-suite facility. 8 wards require patients to share bathroom and toilet facilities. This is mitigated through IPC strategies such as cohorting, dedicated use of a bathroom/ commode as appropriate and enhanced cleaning.
Of the notable achievements, improvements, and extension to secure services facilities at Northside House has increased the number of bedrooms with en-suite facilities in this setting.
Hellesdon site Rivers Centre new wards design will additionally offer an increase in en-suite accommodation for inpatients in the acute adult pathway.
Additional hand hygiene facilities to support infection prevention and isolation zoning in Great Yarmouth Acute Service have been installed.
-
Criterion 8
The Trust is compliant with criterion 8. There is provision of a seven-day access to laboratory support through contracts with the NHS Eastern Pathology Alliance, West Suffolk NHS Foundation Trust, and East Suffolk & North Essex Foundation Trust.
These laboratories link with regional and national networks as required to report notifiable infections and support for further testing.
The Trust has access to a single rapid point of care test (Abbott ID Now) to detect COVID-19 and Influenza infection at ward level.
-
Criterion 9
-
IPC Written Guidance
-
The IPC team produce relevant written IPC policies/ guidance and factsheets to aid clinical staff in the management of infectious patient cases in line with the requirements of the NHS England Board Assurance Framework. These written documents are presented to the IPC committee for consultation for comments and final approval. Following approval, these are available to staff via the Trust intranet site. All documents have version control, author details and date of publication for governance purposes. Monitoring of IPC written documents is completed using a tracker to ensure
these are reviewed within date (maximum 2 yearly) and the compliance is monitored through the IPC Committee quarterly.
An achievement during 2022/23, was the consolidation of many IPC policies into the NSFT IPC Manual which provides written guidance to staff on the expected IPC standards and information on how these standards can be met practically. The NSFT IPC Manual covers the following topics: - IPC Responsibilities; Chain of Infection; Standard Infection Control Precautions (SICPs); and Transmission Based Precautions (TBPs). In addition, 5 other infection specific IPC policies/ guidance were reviewed during 2022/23.
-
IPC & Coronavirus Intranet Site
The IPC team reviewed the IPC intranet site 6 monthly to ensure information available was relevant and up to date.
The IPC team also worked collaboratively with the Communications team to ensure COVID-19 intranet site was reviewed frequently and information was kept up to date as the pandemic progressed into living with COVID-19. Specific COVID-19 Bulletins were also published via email to all staff with regards to important changes such as mask use and testing changes.
-
Compliance with IPC Policies
Monitoring adherence to IPC policies to ensure standards are being met is achieved through the annual IPC audit plan (see appendix 7 for details) which consists of audits conducted by both the IPC team and link IPC nurses (LIPACS).
-
Link IPC Nurse (LIPACS) Audits
During 2022/23 there was very good participation of wards submitting audit data. Overall audit scores were as follows:
-
Mattress – 96%
-
Cleaning – 90%
-
Commode, shower chairs, bath hoists – 94%
Full audit results for audits completed by link IPC nurses (LIPACS) 2022/23 can be found in appendix 7.
Audit results are fed back to individual wards at the time of completing the audit, through a quarterly audit feedback poster which summarises IPC compliance for that quarter and through an annual audit feedback poster which enables wards to see trends of compliance. See appendix 8 for examples.
Where audit results are below the expected standard, these are followed up by the IPC team and relevant ward management team. In addition, the Care Group lead nurses and matrons receive a quarterly IPC summary report to provide oversight on IPC compliance.
-
IPC Team Audits
The IPC team has conducted the following audits during 2022/23:-
-
Water flushing compliance (Monthly) – monitored for returns on usage assessment and flushing recording
-
Hand Hygiene compliance (Quarterly) with an overall compliance score of 92%
-
IPC Mandatory training (Quarterly) – see criterion 6 for details
The IPC team also completed quarterly ward spot checks and a full ward audit for all in-patient ward areas, with results and feedback provided at ward level. In addition, all ECT and clozapine clinics have been audited.
Compliance with IPC in community and outpatient teams has been completed during the COVID-19 pandemic by the Quality & Safety Review teams and at local team level. There is a suite of IPC audit tools that teams can use which is available on the Trust intranet for staff to access. An aim of 2023/24 is for the IPC team to complete audits of all community clinic rooms to assess compliance with standards.
-
Criterion 10
-
Occupational Health Service
NSFT has a contract with the Norfolk & Norwich University Hospital Workplace Health and Wellbeing Service to deliver employment screening, immunisation against communicable diseases and post inoculation exposure management. Trust led quarterly meetings for the review of activity and performance by the contracted service has IPAC nurse representation.
-
Needlestick and inoculation incidents
Needlestick and inoculation incidents which were subject to post incident review to determine root cause and individual assessment and management of those affected was undertaken by the occupational health provider. None met RIDDOR reporting requirements. This number of incidents is a reduction on 2021-22 and is within the range for the previous 4 years’ data.
|
Quarter 1 |
1 contaminated needlestick |
|---|---|
Quarter 2 | 2 contaminated needlesticks |
Quarter 3 | 5 contaminated needles/ sharps incidents |
Quarter 4 | 5 contaminated needlestick/ sharps injuries reported |
-
Fit testing to wear Respiratory Protective equipment (RPE) i.e., a filtering face piece (FFP)
RPE must be considered when a patient with a known/suspected infectious agent/disease spread wholly or partly by the airborne route and when carrying out aerosol generating procedures (AGPs) on patients with a known/suspected infectious agent spread wholly or partly by the airborne or droplet route as per National Infection Control guidance. A fit test is required for every member of clinical staff who will be required to wear this type of PPE for airborne precautions.
Mental Health Trusts are guided to undertake fit testing of their staff as part of ‘best practice’ to meet EPRR Core Standard 12. Face fit testing and RPE user training is recommended by the Health & Safety Executive (HSE) to ensure correct use and seal of RPE, and this test is to be undertaken every 2 years or more frequently if face shape changes. The HSE recommend records to be held at individual level and accessible centrally.
For national and organizational resilience, staff, where possible, are fit tested to 2 different types/brands of FFP3 mask to prevent scenarios of low supply, or skin damage in situations of
prolonged use. FPP3 masks have continued to be supplied to the Trust. There are 7 brands of FFP3 available in the organization. NSFT has initiated the recording of RPE fit test results in ESR for staff substantively employed by NSFT who are within the ESR record system, and all staff receive a ‘Fit Test Passport’ with their test outcome and test date.
The Trust has a substantive post within the IPC team dedicated to the fit testing of clinical staff to wear RPE. The Trust has 4 quantitative method testing machines (portacount equipment).
At end of Quarter 4 of 2022/2023 Trust wide compliance of staff fit tested to least one available brand of FFP3 mask and within two years of fit test was as follows:
441 inpatient clinical staff, 51 NHSP staff, 9 agency staff, 46 students
Activity for 2023/2024 is to offer fit testing on the ‘essential training’ matrix of clinical staff who also train to undertake intermedial life support. Staff will be able to access appointment-based clinics Trust wide to undertake a fit test.
-
Staff vaccination - Seasonal Influenza and COVID-19
The vaccination of healthcare workers against seasonal flu is an annual key action of the Trust winter plan to protect patients, staff and carers against seasonal respiratory illness.
NSFT staff accessed flu and COVID vaccination through local vaccination centres and also NSFT vaccination hubs located in Norwich and Ipswich. Flu vaccine was also administered via peer vaccination routes in the Trust.
The staff vaccination campaign commenced 11th October 2022 and completed 28th February 2023. The IPC team supported the campaign as part of a multidisciplinary vaccination group. The vaccination plan comprised 68 clinics held Trust wide (mix of Flu only, COVID-19 only or Flu/COVID- 19 co-administration), led by IPC with support from Occupational Health who attended at 24 clinics (to administer COVID-19 and/or flu vaccinations). 13 NSFT staff additionally supported as Flu Crew (peer vaccinators).
Uptake for flu vaccine 2022/2023 did not exceed previous years. It was on par with the national percentage uptake. Flu vaccine uptake by frontline staff was 53.7%.
The CQUIN goal for attaining 70%-90% uptake with flu vaccine for frontline clinical staff was not reached. 100% offer of a vaccine was achieved through use of the Vaccination Track system which reminded staff via a weekly email invitation to book an appointment/inform if vaccine received elsewhere/or decline their flu and or COVID-19 vaccination.
Frontline uptake of COVID-19 booster was 61.8%.
Appendices/Supporting Information
Appendix 1 - Abbreviations
|
AMR |
Antimicrobial resistance |
|---|---|
CDI | Clostridioides difficile |
COVID-19 | Coronavirus disease 2019, also known as SARS-CoV-2 |
CQC | Care Quality Commission |
|
Board of Directors 23 November 2023 Annual Director of Infection Prevention and Control (DIPC) Report 2022/23 |
Version 1 |
Author: Elaine Thrower & Natalie Wilkin Department: Infection Prevention & Control Team |
|---|---|---|
Page 20 of 27 | Date produced: June 2023 | Retention period: 20 years |
|
DHSC |
Department of Health and Social Care |
|---|---|
DIPC | Director of Infection Prevention and Control |
E Coli | Escherichia coli |
ESBL | Extended Spectrum Beta Lactamase |
HCAI | Health Care Associated Infection |
IPC | Infection Prevention & Control |
MRSA | Methicillin Resistant Staphylococcus Aureus |
NSFT | Norfolk and Suffolk Foundation Trust |
PLACE | Patient-led assessments of the care environment |
PPE | Personal protective equipment |
RCA | Root Cause Analysis |
Appendix 2 - IPC Code of Practice Table
|
Criterion |
Detail |
|---|---|
1 | Systems to manage and monitor the prevention and control of infection. These systems use risk assessments and consider the susceptibility of service users and any risks that their environment and other users may pose to them. |
2 | The provision and maintenance of a clean and appropriate environment in managed premises that facilitates the prevention and control of infections. |
3 | Appropriate antimicrobial use and stewardship to optimise outcomes and to reduce the risk of adverse events and antimicrobial resistance. |
4 | The provision of suitable accurate information on infections to service users, their visitors and any person concerned with providing further social care support or nursing/medical care in a timely fashion. |
5 | That there is a policy for ensuring that people who have or are at risk of developing an infection are identified promptly and receive the appropriate treatment and care to reduce the risk of transmission of infection to other people. |
6 | Systems are in place to ensure that all care workers (including contractors and volunteers) are aware of and discharge their responsibilities in the process of preventing and controlling infection. |
7 | The provision or ability to secure adequate isolation facilities. |
8 | The ability to secure adequate access to laboratory support as appropriate. |
9 | That they have and adhere to policies designed for the individual’s care, and provider organisations that will help to prevent and control infections. |
10 | That they have a system or process in place to manage staff health and wellbeing, and organisational obligation to manage infection, prevention and control. |
Appendix 3 - IPC Team Structure
Appendix 4 - IPC Committee Governance Reporting Structure
|
Board of Directors |
|---|
Quality Assurance Committee |
Quality Committee |
Infection Prevention & Control Committee |
Appendix 5 - COVID- 19 Infection Data (2022/23)














Appendix 6 - Norovirus Infection Data (2022/23)









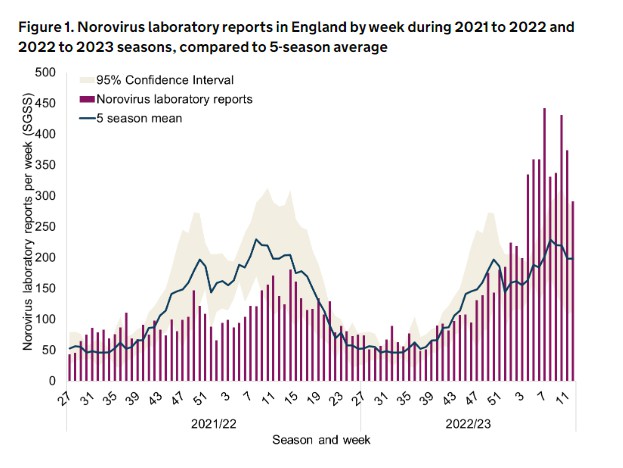 UK
Health Security Agency (UKHSA) surveillance data for comparison
UK
Health Security Agency (UKHSA) surveillance data for comparison
Appendix 7 - 2022-23 Audit Programme & Compliance Scores
|
Compliance Scores |
|||||
|---|---|---|---|---|---|
Audit Type | Frequency | Q1 | Q2 | Q3 | Q4 |
Mattress | Quarterly | 96% | 97% | 97% | 94% |
Cleaning & Disinfection | Quarterly | 92% | 92% | 90% | 85% |
Commode, shower chairs, bath hoists | Quarterly | 93% | 92% | 96% | 95% |
Hand hygiene | Quarterly | 93% | 93% | 89% *Limited data | 93% |
Water flushing | Monthly | Compliance scores not applicable – individual reports & feedback given to teams directly. Compliance scores monitored by IPC team on audit tracker. | |||
IPC Nurse Ward spot-check visit | Minimum quarterly | ||||
ECT Suites | Annual | ||||
Clozapine Clinics | Annual |
Appendix 8 – Example of Audit feedback poster provided to wards


Quarterly feedback
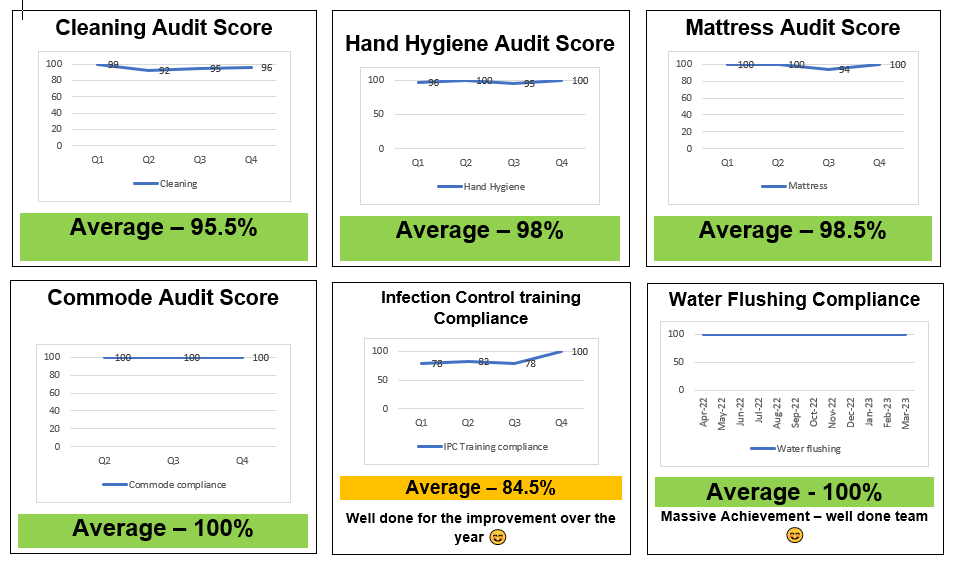 Annual Summary
Annual Summary
Appendix 9 – Hydrop Ltd. Audit findings September 2022
|
ASSESSED LEVEL OF OVERALL GOVERNANCE ASSURANCE |
||
|---|---|---|
CURRENT ASSURANCE INDICATOR | GENERAL NOTES | |
REASONABLE ASSURANCE |
| Internal control, no matter how well designed and operated, can provide only reasonable and not absolute assurance regarding the achievement of the organisation’s objectives. The likelihood of achievement is affected by limitations inherent in all internal control systems. These include: the possibility of poor judgement in decision-making; human error; control processes being deliberately circumvented by employees and others; management overriding controls; and the occurrence of unforeseeable circumstances. Where a control objective has not been achieved, or where it is viewed that improvements to the current internal control systems can be attained, recommendations have been made that if implemented, should ensure that the control objectives are realised/ strengthened in future. A basic aim is to provide proactive advice, identifying good practice and any systems weaknesses for management consideration. It is accepted that, Legionella bacteria colonies can be present randomly in a water system, since they are considered to be ubiquitous. The presence of the bacteria is also considered to be possible even in systems which are well managed and maintained, albeit under a reduced potential of colony proliferation. |
PREVIOUS ASSURANCE INDICATOR | ||
REASONABLE ASSURANCE |
| |
INDICATOR | ASSESSED LEVEL OF OVERALL GOVERNANCE ASSURANCE | |
|
|
|
|
|---|---|
|
|
|
|
|
|
|
Date: |
23rd November 2023 |
L |
|---|---|---|
|
Item: |
23.58 |
|
Report To: |
Board of Directors |
|---|---|
Meeting Date: | 23rd November 2023 |
Subject of Report: | Annual Research & Development Report |
Purpose: | For assurance |
Author: | Bonnie Teague Job title: Head of Research Jon Wilson Job title: Research Director |
Director: | Alex Lewis, Interim Chief Medical Officer |
Legislation/Compliance | NIHR Clinical Research Network High Level Objectives CQC Well-led Indicators W8.1, W8.5. |
How this paper impacts on Trust Strategic Objectives | Exceptional care - through generating and sharing an evidence-base for our care decisions and service design. Transforming Lives - through co-production, design and development of research which meets the needs of our population and involves representatives at each stage of the research cycle. Working collaboratively with partners across the region, nationally and globally and supporting our healthcare professionals and partners to engage in research, evaluation and evidence-finding. |
Executive Summary:
This report contains the annual update of current Research Performance, Activities and Service Improvement initiatives taking place in the Research Department.
-
840 participants recruited into national research studies compared to a target of 730.
-
No critical findings identified from Research audits.
-
New National and global research and implementation grants have been awarded in 2023-24.
-
A new Quality and improvement Outcome Framework (QIOF) for NHS Library Services has been introduced, with NSFT being reviewed in February 2024.
-
The team has won a national Innovation award for its project evaluating digital technologies for child anxiety and a regional Innovation award for a nursing research programme.
Risks identified:
-
Changes in research funding models may mean reduced research income in future years.
-
Lack of resources means there is a risk that non-funded services provided to NSFT staff such as evaluation support, trust programme support, training and supervision may need to be reduced
Actions being taken:
-
Business plan for increased funding in development.
-
Request for clinical trial facilities on the Hellesdon site redevelopment.
Recommendations:
-
To note the annual report
-
Background:
This paper is submitted by the Research and Development Department, on behalf of the NSFT Research Committee summarising quality and performance across 2022-23 and from April- September 2023.
The purpose of the NSFT Research Committee is to provide an approval and oversight committee of all Research Activities in the Trust. This includes policy approval, Performance reporting, Safety reporting, reports from Delivery and Development teams, and updates/actions from partner organisations. Committee members have continued submitting reports throughout 2022-23 prior to a virtual meeting each month.
This report is submitted in order to detail the current work and assurance oversight of the Research Department. It is to provide updates to the Quality Assurance Committee and to escalate any identified areas of risk and to request support or decision making where required.
-
The NSFT Research Department includes three distinct teams:
-
Research Delivery: A multi-disciplinary team of specialist research nurses, AHPs and support staff which promotes and delivers approved national and international research studies to NSFT service users and carers. The types of research delivered range from drug trials and therapy interventions to observational work.
-
Research Development: A team of clinical researchers which works with clinical teams, academics, service users and carers to identify areas of clinical need in order to develop high-quality research proposals for grant funding. The team also advises clinical teams about undertaking evaluation projects and disseminates research outcomes through high- impact publications.
-
Library Services: A specialist mental health team providing clinical teams with access to the latest evidence and knowledge to inform clinical practice and decision-making.
-
Main Report:
-
Research Delivery Performance:
Clinical Research Network East of England has annual performance indicators, called High Level Objectives, for each partner organisation. The following activity areas are subject to reporting requirements from NSFT to the CRN: overall recruitment numbers, efficient study delivery (predicted delivery to time and target of open studies) for Commercial and Non-Commercial activity, and Participant Experience Feedback Engagement (PRES).
Funding from CRN East of England to NSFT reduced by 5% in 2023-24 due to lack of Commercial/Industry activity. A new funding model is proposed from April 2025 after the new regional research delivery networks (RRDN) are launched in October 2024 as a replacement for the CRN, however this is expected to continue the emphasis on Commercial activity.
We have reorganised the structure of the delivery team to meet increased activity and support transition of leadership roles, including a new Research Manager and new Lead Research Nurse.
Recruitment Performance
-
In 2022-23, NSFT recruited 840 participants into national CRN research (non-COVID) compared to a target figure of 730. This marked a return to pre-pandemic activity levels. By September 2023, we have recruited 343 since April, which is a little above last year’s performance rate and is higher than multiple partner organisations.
-
The % of open non-commercial studies predicted to recruit to time and target is recovering after the pandemic, although more work needs to be done to reach the 80% target (currently 63%).
-
We have met target for the submission of number of PRES (experience surveys) to the CRN in 2022-23 and 2023-24.
-
No Commercial research was started in NSFT in 2022-23, so this objective was not achieved. 6 Expressions of Interest have been submitted, but NSFT has not been selected as a site.
-
Research Safety Oversight:
-
Research Audits
Research audits have continued through 2022-23 and 2023-24 to examine compliance with HRA ethically approved procedures and ICH-GCP conduct standards. No research audits have led to the identification of critical findings or failures, with one major finding relating to lack of oversight of staffing responsibilities in Suffolk. Self-audit reports have been completed by all research teams with no major findings.
Safety - Adverse Events
9 Serious Adverse Events were received for in-patient hospitalisations and participant deaths in 2022-23, and 6 so far in 2023-24. No serious adverse events were related to the research activity.
26 adverse events (non-serious adverse events) have been reported and managed appropriately.
17 adverse events have been reported so far in 2023-24. No reports were attributable to the conduct of studies.
Wellness support checks have led to 7 referrals to partner organisations for financial and/or psychological support.
-
Service Evaluations:
49 service evaluations have been reviewed and approved by NSFT Research in 2023 so far. As part of a Quality collaborative with QI, Library and Clinical Audit departments, we are compiling an abstract book of all quality work undertaken in NSFT, ready for dissemination in April 2024. We are hoping this will become an annual record of NSFT’s quality project activity going forward.
-
Research Development:
We have obtained new research grant funding from the National Institute for Health and Social Care Research for the CHERISH project (Community engagement in research) with the University of East Anglia and a Fellowship from the NICHE Institute (Norfolk Coastal and Rural Health Inequalities). We are awaiting outcome on 2 further NIHR grants that have been submitted in the area of eating disorder support and intergenerational mental health. There are multiple large-scale grants in development for submission in 2024.
In 2023, the team was awarded its first global health collaborative project from the Canadian Institute of Health with our partners at the University of Ottawa, to co-design and validate a global patient-reported experience measure of mental health diagnosis in English and French.
NSFT received its first implementation evaluation project funded by the Mental Health Innovation Network (MHIN). This work is aiming to implement and evaluate parent-delivered CBT across multiple schools in Norfolk and Suffolk. The project has just secured continued funding throughout 2024.
We are increasingly working with regional partner organisations as collaborators on small-scale regional research projects, including the NNUH on digital solutions to support the holistic needs of children attending excess weight clinics (TOSCA), and Norfolk County Council on a new climate- related project to support psychological resilience in Norfolk coastal communities (RIPPLE).
A number of studies have now been completed and their final reports approved by the NIHR. For a list of the core activities and studies of the Research Development team, please see Appendix 1.
-
Library Services Update:
-
Quality and Improvement Outcomes Framework Background
-
As part of the wider Quality Framework for NHS organisations in receipt of funding through the NHS Education Contract, NSFT is required to ensure that there is a proactive, high-quality knowledge and library service that is available to all staff and learners. Evidence to demonstrate compliance is a requirement of the Quality and Improvement Outcomes Framework (QIOF) for NHS-Funded Knowledge and Library Services in England (NHS England, 2022).
The QIOF is a rolling process on a three-year cycle. Between 2023/24 and 2025/26 every NHS organisation is required to submit evidence, NSFT has been timetabled to submit in 2023/24.
There are six QIOF outcomes, five levels within each ranging from Not Met to Excellent, there are 61 indicators across the six outcomes.
Evidence has been gathered prior to NSFT’s submission in January 2004, the evidence includes:
-
A service improvement plan for two outcomes identified with input from NHS England.
-
NSFT Library Services annual report
-
NSFT Library Services strategy
A review meeting will be held with NHS England in February 2024, NSFT’s representatives will include the library services manager, the head of research and at least one other representative – quality education lead/trust director - responsible for library services.
-
NSFT Library Services impact survey 2023
In August 2023, a survey was conducted to provide an insight into the impact of library services on NSFT staff and services. 123 members of NSFT staff who had accessed one or more library services/resources in the previous 12 months were invited to complete the survey, 51 responses were received, a response rate of 41%.
Key findings:
-
NSFT staff predominately access library services for personal/professional development, to inform personal practice/knowledge and direct patient care.
-
NSFT staff routinely share knowledge and learning they have gained from accessing library services formally and informally with their colleagues.
-
NSFT staff value highly the physical and remote/online services and support provided by NSFT library services.
The findings demonstrate that accessing NSFT library services encourages a culture of shared learning and knowledge within the trust. Knowledge derived from accessing NSFT library services
is disseminated widely to colleagues and teams and is informing up-to-date and best practice. Informed decisions improve outcomes, quality of care and patient experience.
-
Research Outputs and Impacts:
-
The I-DIGIT Research team led by NSFT Research, which was evaluating digital technologies for child anxiety, won a national Innovate Award from NHS England for Outstanding Contribution to Population Health Through Innovation in September 2023. This work has also been shared across multiple national webinars.
-
The team won a regional ‘Innovation and Improvement’ award from NIHR Clinical Research Network for its nursing research and teaching programme with the University of East Anglia.
-
Training relating to research quantitative and qualitative methodologies, clinical research in practice, informed consent, statistical analysis and critical appraisal has been delivered to 165 NSFT staff in 2022-23.
-
In 2023, we ran our first Research Summer School, engaging under-served young people to train and undertake research, and support their psychology and nursing university applications.
-
NSFT has been invited by the WHO to a global meeting in November 2023 to discuss ICD-11 and mental health diagnosis with our partners at the University of Columbia and Ottawa.
-
The 3rd Annual Research Seminar took place in June 2023, opened by Zoe Billingham. 145 people attended to hear about the latest in NSFT-led research.
-
NSFT Research nurses had their work accepted for presentation at two national conferences in 2023-24, including the International Nursing Research and the National Health and Social Care conference.
-
We have also been invited to be part of a group travelling to Vietnam in December to support healthcare students in understanding mental health and climate change.
-
There have been 21 peer-reviewed journal publications with NSFT authors published since April 2023.
-
-
Impact on people who use services and their carers
We have responded to last year’s PRES survey data to revise our Research welcome packs with clearer information about research processes and other research opportunities and have also started to develop new welcome and support materials for people living with dementia and their carers.
-
Equality implications
We undertake an evaluation of our research referrals system (REACH) each year to establish our performance on key demographic characteristics: gender, age, ethnicity, deprivation and disability status as compared to the Norfolk and Suffolk population. We have found that we have good reach into deprived areas and people with disabilities, but how lower representation from younger children and ethnic minority groups. Since last year’s evaluation, we have created new research opportunities for younger children and received additional funding for the inclusion of under-served
groups in NSFT-led research studies to ensure equitable representation, and to examine some of the structural barriers facing groups with additional needs in health services.
In addition, we are supporting a number of health trainee research and evaluation projects in a programme of health and mental health inequalities for different ethnic and cultural minority groups, social class and coastal and rural deprivation.
-
Financial implications
-
Currently no funding is received from NSFT to support the research delivery or development teams, which are both dependent on limited external funding only. Additional resource is needed to support growing number of Trust programme evaluation requests, as current team are at capacity. There is a risk not being able to support future evaluation work, improvement initiatives, training or maintain income on development programme, due to overcommitted resources.
-
A business plan is in the early stages of development to support this continued work, and to develop and fund a Centre of Research Excellence to broaden training and development opportunities.
-
Risks Identified:
-
The current CRN funding contract finishes on 31st October 2024, although funding is expected to continue beyond this date using a new model. Currently we are experiencing a 5% year on year cut to the Research delivery budget, as well as not been awarded additional funding to the Development team, due to the lack of Commercial income. If this model continues, we could lose our core funding within a few years.
-
Our ability to attract Commercial research to NSFT is significantly hampered by the lack of clinical research facilities on the Hellesdon site which is needed due to contractual requirements relating to proximity to pharmacy, and the need to be easily accessible to medic investigators on site who are required to be involved in commercial clinical trials. We have requested these facilities in the site move as a matter of operational urgency, but are still awaiting an update.
Appendix 1: Research Development Team Activity
|
Short Grant name |
Area of Focus |
Duration |
Funder |
Amount |
Submitted |
Funded, In Set-up |
Active |
Submitted/Completed |
|---|---|---|---|---|---|---|---|---|
BEST | Young people's mental health care in schools | 2 years | NIHR | £351,000 | ||||
ICALM | IPC for Adolescent mental health | 3 years | NIHR | £381,000 | ||||
IACT4CARERS 1 | ACT for Carers of people with dementia | 2 years | NIHR | £208,000 | ||||
ASPIRE | Developing a Parent-supported positive psychology model for children with adverse life experiences | 18 months | NIHR | £148,000 | ||||
LIMITLESS | Supporting Young people in Care through lifestory work | 18 months | NIHR | £143,000 | ||||
I-DIGIT | Technologies to support Child anxiety | 15 months | NIHR | £130,000 | ||||
MINDS | Improving Adult mental health discharge from wards | 3 years | NIHR | £973,000 | ||||
DISCOVERY | Post-diagnostic support for people with dementia | 3 years | NIHR | £693,000 | ||||
Diagnosis Experiences | Understanding experiences of mental health diagnosis in adults in UK and Canada and developing a diagnostic PREM | 2 years | CIH | £70,000 | ||||
ANSWERS | Understanding young people's needs during COVID recovery | 12 months | UEAHSCP | £23,000 | ||||
TOSCA | Developing TechnOlogy to Support ChAnge (TOSCA tudy) for young people and their families seen in the complications of excess weight service (with NNUH) | 12 months | UEAHSCP | £15,000 | ||||
CARECOACH | Supporting Carers of people with dementia | 5.5 years | NIHR | £1,920,000 | ||||
WoW | Evaluating implementation of parent-delivered CBT | 14 months | NIHR MHIN | £75,000 | ||||
CHERISH | Community engagmeent in health behaviour research | 18 months | NIHR | £147,000 | ||||
RIPPLE | Supporting Norfolk communities to improve psychological preparedness for climate-related flooding events (With NCC) | 12 months | UEAHSCP | £20,000 | ||||
LINEAGE | Co-designing a hybrid psychoeducation resource for non-custodial grandparents of young people seeking, waiting for, or accessing mental health services (LINEAGE) | 18 months | NIHR | £148,000 | ||||
ALLIANCE | A Realist Synthesis to Ground Improvement of Trust and Therapeutic Relationship between Service Users and Healthcare Staff in the Inpatient Treatment of Eating Disorders: ALLIANCE study | 18 months | NIHR | £145,000 |

|
Report To: |
Board of Directors |
|---|---|
Meeting Date: | 23rd November 2023 |
Title of Report: | Chair’s report of the Performance and Finance Committee meeting held on 15th November 2023 |
Purpose of report: | For Assurance |
Author: | Adrian Matthews, Non-Executive Director |
Director: | Zoë Billingham, Chairperson |
Link to BAF / Risks | BAF risks relevant to Committee’s work – see end |
Executive Summary:
This report provides an update to the Board on the meeting of the Performance and Finance Committee held on the 15th November 2023.
Recommendation
The Board is requested to note the assurance and continued scrutiny examined by the Committee during its meeting.
Performance and Finance Committee 15th November 2023 Positive Assurance
-
In Part 1, the Committee received a detailed update on the progress of the operational review of Crisis Resolution and Home Treatment Teams. This is very much the front line of the Trust’s response to members of our community who are in crisis and need immediate help and support. The pressure and workload on our five teams has increased significantly as demand for mental health services has risen. The operational offer by the Trust has not kept pace with this demand, and the review, whilst not yet complete, is a root and branch study of what the service does well and what it does not do well. When complete, the report will identify a reconfigured service provision which has been designed with service user, carer, and stake holder involvement to focus the response to those who need our immediate help, with more effective and timely response.
-
For some time, the Committee has discussed the ongoing demand and capacity project. Mostly this has seen small pockets of progress, but with one or two significant pieces of work such as within Children’s and Young People’s services in Suffolk. However, the report identified a significant shift in the process with evidence that operational teams are now not only engaged with the planned projects but are approaching the demand and capacity team for specific pieces of work to be done within their teams. This move from a “push” to a “pull” in this process takes this work to a new level, as teams have identified that this process is needed to help identify demand pressure, lack of or poorly focussed capacity, or gaps in the productivity of operational delivery. As this process is embedded it will become the foundation of many stands of work that is undertaken to transform services, and drive effectiveness and efficiency.
Decisions Made
-
The Committee received the annual report and accounts 2022/23 for the charitable funds. These were agreed and are recommended to the Board for approval.
-
The Committee discussed the emerging Estates Strategy. This is a key supporting strategy to the refreshed Trust strategy. This is still a work in progress and the Committee were requested to offer feedback. The strategy was agreed in principle, with the allowance of Chair’s action to agree the strategy should this be required before it is recommended to the Board for approval.
-
Similarly, the Committee also reviewed the revised Digital Strategy. Unlike the Estates Strategy, this is an updated strategy so is significantly more complete. Whilst more work is required, again, the Committee granted the use of Chair’s action if this is required before it is recommended to the Board for approval.
-
The Committee agreed the submission of the second half year iteration of the financial plan. It is not proposed that there will be any amendments to the original plan that was previously agree by the Board.
Matters of Concern and Key Risks to Escalate
-
Without being repetitive, the Trust’s financial position is still a significant cause of concern. Whilst the Committee approved the plan to breakeven, this is being supported by one-off non-recurrent efficiency plans. This is not sustainable. The breakeven forecast for March 2024 leaves the Trust with an underlying deficit of £12.8m. To put this into perspective, this is approximately 3.75% of the Trust’s income. It is essential that the Trust gets to grip with this deficit and begin to erode it with recurrent efficiency programmes. Inflation remains extremely high, pay awards will continue to be part funded by Government, and overall public finances will continue and become even more stretched. These things together are likely to worsen the position, not support it to get better. Therefore, the only solution is for the Trust to generate efficiencies by transforming services that are more focussed on patient need, totally effective, less wasteful of precious resources, and efficient.
-
The Committee received an update on the deep dove process that is being undertaken within Children’s and Young People’s service in Norfolk and Waveney to understand the root cause and identify solutions to the waiting lists. There are early signs that this forensic focus on the waiting lists could see ideas and solutions to this problem. However, the deep dive report will not be complete and will not report until the January Committee. As this deep dive has been commissioned by all Committees of the Board, it is important that all committees are able to receive and discuss the findings. In the meantime, waiting lists in these services remains a major risk for the organisation.
Major actions commissioned / work underway.
-
See update above of the Committee commissioned deep dive into waiting lists.
-
The Committee received an update into the review and repurposing of the Quality Performance Meetings (QPMs). These Executive led meeting are an essential conduit to manage performance within the organisation, hold senior leaders to account and provide the governance to drive quality improvement through the organisation. The Committee plays a key role in ensuring this new process delivers on its aims, quickly and efficiently. Reports from the QPMs will form a major part of how the Committee will gain assurance that accountability for performance is being delivered throughout the organisation.
Strategic Objective – Exceptional care
Risk Description 2.3 – risk that growing waiting lists result in deteriorating access to timely and effective care, impacting patient safety. Risk Appetite – the Trust has a very low/averse appetite for risks that impact on quality, safety and patient experience
Date last reviewed:
November 2023
Director Lead:
Thandie Matambanadzo, Chief Operating Officer
Board Committee: Performance and Finance Committee
Consequence of risk:
If waiting lists continue to grow, then people are unable to access timely care and treatment impacting on patient safety, outcomes and experience.
Target Rating: (l x c) and Date to reach target
Target rating 3 x 3 by March 2025
Risk Rating over time
25
15
5
Rationale for current score: (l x c): waiting lists waiting lists remain high since the pandemic reflecting national trends, exceeding risk appetite and representing a significant and ongoing risk to service users.
Controls (what are we currently doing about the risk?)
-5 Jan-23 Mar-23 May-23 Jul-23 Sep-23 Nov-23
Assurances (how do we know if the things we are doing are having impact?)
-
Trust-wide service user tracking list (SUTL) process implemented with all care groups expected to provide monthly report to a Trust Access Group (TAG), with escalation process and reporting.
-
Following implementation of SUTL processes, care groups will be asked to provide information on compliance with clinical harm review processes (from November 2023).
-
A “deep dive review” has been commissioned by non-executive directors into waits within children, families and young people’s services within Norfolk and Waveney. The review will be completed by January 2024 and include a recovery and improvement action plan (an initial draft of the review has been completed).
-
Monitoring of key operational metrics reported in quality & performance meetings (QPMs) and via Integrated Quality Performance Report (IQPR)
-
Patient flow measures introduced and routinely reviewed at governance forums including a focus on system working on delayed transfers of care (DTOC), urgent & emergency care (UEC) programme and community transformation programmes in Norfolk and Suffolk.
-
TAG reviewing care group status reports on long waits, performance against agreed recovery/improvement plans and assurance around local clinical harm review processes in place. TAG escalating issues to QPMs and where necessary to performance and finance committee by the COO. The first TAG meeting was held on 31 July 2023 and the last meeting took place on 30 October 2023.
-
IQPR) metrics
-
The Trust are seeing sustained improvement trends in referral to assessment and treatment for adult community waits across the Trust. Children and young people’s services continues, however, to be disproportionately affected by excessively long waits especially in Norfolk and Waveney.
-
Reflecting global trends, we continue to see an exponential growth in waiting lists for neurodevelopmental conditions including for ADHD and ASD. The Trust is working with both ICB's to identify system-wide interventions in this area. A position paper is also being prepared in this area for the Trust executive group.
-
Patient flow interventions currently being planned/deployed including system working on delayed transfers of care (DToC), urgent and emergency care (UEC) and community mental health transformation programmes across Norfolk and Suffolk. Interventions are underway for out of area placements including strengthening senior clinical decision- making and providing visibility of data across leadership teams.
|
|
|---|---|
Gaps
carrying high occupancy rates. | Mitigating actions (what have we done/what more should we do?)
|
Strategic Objective – Creating the conditions and environment to achieve Risk Description 4.1 Risk of lack of access to timely and good quality data to enable effective decision-making and improvement.
Risk Appetite: The Trust has a very low/averse appetite based on the impact of poor data quality on quality, safety and patient experience.
Date last reviewed:
November 2023
Director Lead: Thandie Matambanadzo, Chief Operating Officer
Board Committee:
Performance and Finance Committee
Consequence of risk:
If data quality is poor, then this negatively impacts our ability to provide meaningful and accurate information to enable effective decision making and safe services for our services users and performance management information
Target Rating: (l x c) and Date to reach target
Target rating 3 x 3 by March 2025
Risk Rating over time
25
20
15
10
5
0
Rationale for current score: (l x c):
Better scrutiny and continued improvement with data quality but more work needed on clinical support and inputting on Lorenzo for accurate recording.
Controls (what are we currently doing about the risk?)
-
Integrated quality and performance report (IQPR)
Jan-23 Mar-23 May-23 Jul-23 Sep-23 Nov-23
Assurances (how do we know if the things we are doing are having impact?)
-
Regular reports on data quality to performance and finance committee alongside
-
The Business Change teams manage Standard Operating Procedures (SOPs) related to data entry on Lorenzo.
-
Check and challenge at local governance meetings and then at quality and performance meetings (QPMs).
-
Access, Data and Delivery improvement programme pillar work
-
Guides and team support for using Lorenzo.
-
Electronic patient record (EPR) re-procurement commenced with clinical engagement and programme management support
-
Training teams on Making Data count, PowerBI etc
-
Data Quality Risks and Issues Log implemented to evidence key risks
Gaps
-
Lack of clinical and medical presence at key meetings that can help improve Data Quality.
-
Ensuring staff are utilising the training so they are better prepared to make use of data to inform decision making.
-
System changes that can alleviate Lorenzo constraints to better enable staff to capture and access data
IQPR
-
IQPR continues to develop and is routinely being used for analysis and decision- making about improvement priorities and is leading to demonstrable data quality improvements and highlighting specific data quality issues at service level.
-
Improved QPMs, with NED attendance, providing a mechanism for checking, challenging and supporting care group leadership teams to deliver on quality and performance objectives including improving data quality. However, there is more to do to ensure that local governance meetings and systems are aligned to ensure ‘floor to board’ reporting at service level.
-
The Data Quality Group has been reinstated and discusses key and emerging data quality risks and issues.
Mitigating actions (what have we done/what more should we do?)
-
A Data Quality policy is being prepared, as part of pillar work, with plans to present to the executive group and onwards to the performance and finance committee
-
A Data Quality Day was held in Norwich on 18th October to focus on our top risks and issues. Over 50 clinical, admin and corporate staff attended the collaborative problem-solving workshops to understand why these issues occur and to agree sustainable actions that would help make a difference
|
|
|---|
|
Strategic Objective 4 – Creating the conditions and environment to achieve |
|||
|---|---|---|---|
Risk Description 4.2 Failure to maintain financial sustainability Risk Appetite – the Trust has a low appetite for risks that impact on financial sustainability, but moderate appetite where this helps deliver substantial benefits to service users and/or realises significant longer-terms efficiencies | Date last reviewed: November 2023 | Director Lead: Jason Hollidge, CFO | Board Committee: Performance and Finance Committee |
Consequence of risk: If the Trust is not able to maintain financial sustainability, then, it will not have sufficient funds to provide the services required to the population we serve, or be able to invest in service improvements in the future, or meet statutory financial duties leading to tighter external control | Risk Rating over time 25 20 15 10 5 0 Jan-23 Mar-23 May-23 Jul-23 Sep-23 Nov-23 | Rationale for current score: (l x c) Submitted break-even plan for 2023/24, M6 performance in line with plan including break- even forecast out-turn, however, mitigations of the underlying overspend position within 2023/24 are non-recurrent in nature High Risk 5 x 5 = 25 | |
Target Rating: (l x c) and Date to reach target 1 x 4 = 4 March 2024 | |||
Controls (what are we currently doing about the risk?)
| Assurances (how do we know if the things we are doing are having impact?)
|
|
underlying break-even position by 2028/29, based on current assumptions. |
|
|---|---|
Gaps
| Mitigating actions (what have we done/what more should we do?)
|
|
Strategic Objective 4 – Creating the conditions and environment to achieve |
|||
|---|---|---|---|
Risk Description 4.3 Risk of failure to deliver Rivers Centre new build Risk Appetite – the Trust has a moderate appetite to the new build | Date last reviewed: November 2023 | Director Lead: Jason Hollidge | Committee: Performance & Finance Committee |
Consequence of risk: If we fail to build and deliver the new Rivers Centre build on time, on budget and without appropriate therapeutic environment, this impacts on our ability to deliver quality of care, reduce out of area and reputation impact | Risk Rating over time 20 10 0 Jan-23 Mar-23 May-23 Jul-23 Sep-23 Nov-23 | Rationale for current score: (lxc) Construction programme progressing well on site. Weather having a minor impact but buildings will be weather tight from December 2023 onwards. Major Risk 3 x 4 = 12 | |
Date to reach Target Rating: (l x c) long term risk, expect to reduce risk at each gateway approval stage - 1 x 3 = September 2024 | |||
Controls (what are we currently doing about the risk?)
| Assurances (how do we know if the things we are doing are having an impact?)
| ||
Gaps
confirmed. | Mitigating actions (what have we done/what more should we do?)
|
|
Report to: |
Board of Directors |
|---|---|
Meeting date: | 23rd November 2023 |
Title of report: | Charitable Funds Annual Report and Accounts 2022-23 |
Purpose of paper: | For approval |
Author: | Sarah Ruffles, Assistant Financial Accountant |
Director: | Jason Hollidge, CFO |
Link to Trust Strategy | Exceptional care |
Legislation/Compliance | NHS Charities Compliance |
Link to BAF Risk/s | BAF risk 4.2 |
Executive Summary:
The purpose of this paper is to present the Norfolk and Suffolk NHS Foundation Trust Charitable Funds 2022/2023 Annual Report and Accounts.
The Performance and Finance Committee reviewed the Annual report and accounts at its meeting on 15th November 2023 and recommended to the Board for approval.
Recommendation:
The Board is asked to review and recommend approval of the Annual Report and Accounts for the Norfolk and Suffolk NHS Foundation Trust Charitable Funds for the 2022-23 financial year.
-
Accounts Overview – Income and Expenditure
The level of charitable income from voluntary donations and legacies received in the year was
£39k, an increase of £14k compared to 2021-22 (£25k). Total expenditure for the year was £39k (£74k in 2021-22).
Administrative and support costs including the Independent Examiner’s fee have been borne by the Trust due to a lack of investment income or interest from cash deposits during the year which has traditionally been used to fund these costs.
-
Accounts Overview – Balance Sheet
Total funds decreased by £16k during the year due to the reduction in funds received and continuation of expenditure in year.
No funds were closed during the year.
-
Approval of the Annual Report and Accounts
The accounts have been compiled in accordance with the relevant accounting standards and have been reviewed by Ensors Accountants LLP. The independent Examiner’s report is included within the Annual Report.
The Chair of the Trust and one other Trustee will be required to sign off the Accounts at a Board of Directors meeting prior to submission.
Following the Board’s approval, the accounts will be signed by the Independent Examiner and submitted to the Charity Commission on or before the final deadline of the 31 January 2024.
Charitable fund and other related charities
Annual report and accounts
1st April 2022 to 31st March 2023
Corporate Trustee:
Norfolk and Suffolk NHS Foundation Trust Registered address:
Hellesdon Hospital Drayton High Road Norwich
NR6 5BE
Registered Charity Number: 1103563
Created by the governing document, the Trust Deed, dated 1 April 2004
 Norfolk
and Suffolk NHS Foundation Trust Charitable Funds Annual Report 1st
April 2022 to 31st March 2023
Norfolk
and Suffolk NHS Foundation Trust Charitable Funds Annual Report 1st
April 2022 to 31st March 2023
Contents
| 4 – 5 | |
|---|---|
| 6 – 9 | |
Statement of Responsibilities of the Corporate Trustee | 10 |
Independent Examiner's Report | 11 |
| 13 | |
| 14 | |
| 15 | |
| 16 – 25 |
Corporate Trustee and Advisers
Corporate Trustee
Norfolk and Suffolk NHS Foundation Trust is the sole Corporate Trustee, with members of the Trust’s Board acting as ex-officio trustees of the Charitable Funds.
The Board of Directors of Norfolk and Suffolk NHS Foundation Trust who served during the financial year were as follows:
Chair
Zoe Billingham
Non-Executive Directors
Tim Newcomb Pip Coker
Ken Applegate Adrian Matthews
Katy Steward (to 30.09.22) Patricia Fuller
Lindsey Hoy
Dr Roger Hall (from 05.12.22) Sally Hardy (from 09.01.23)
Executive Directors
Stuart Richardson – Chief Executive
Cath Byford – Deputy Chief Executive and Chief People Officer (from 09.05.22)
Daryl Chapman Chief Finance Officer (to 03.01.23)
Jason Hollidge – Chief Finance Officer (from 03.01.23)
Diane Hull – Chief Nurse (to 31.07.23) Amy Eagle – Interim Chief Operating
Officer (to 11.05.22)
Tumi Banda – Interim Chief Nursing Officer (from 10.07.23)
Kathryn Ellis – Chief Strategy, Improvement and Partnership Officer
Thandie Matambanadzo – Chief
Membership
-
A Non-executive Director will chair the Committee.
The membership of the Committee shall be:
-
Non-executive Director (Chair)
-
The Chief Finance Officer (or delegated nominee)
-
Company Secretary
All committee members may delegate a suitable representative.
-
Nominated Representatives:
Norfolk and Suffolk NHS Foundation Trust
-
Adrian Matthews
-
Daryl Chapman – Chief Finance Officer (to 03.01.23)
-
Jason Hollidge – Chief Finance Officer (from 03.01.23)
-
Jean Clark - Company Secretary
-
No business shall be transacted at a meeting of the Charitable Funds Committee unless at least three representatives are present.
Charitable Funds Committee attendance 2022/23
19 16
July November 2022 2022
Adrian Matthews
Operating Officer (from 11.05.22) Daniel Dalton – Chief Medical Officer (to
31.07.22)
Alex Lewis – Chief Medical Officer (from 01.08.22)
The Corporate Trustee has delegated, within written terms of reference, day to day management of the funds to the Charitable Funds Committee. The Committee is now incorporated into the Trust’s Finance, Business and Investment Committee.
The Committee operates with the following membership:
Non-executive Director Daryl Chapman
Chief Finance Officer Jean Clark
Company Secretary
🗸 🗸
🗸 🗸
🗸 🗸
Registered Address
The Registered Office of the Charitable Fund is:
Norfolk and Suffolk NHS Foundation Trust Hellesdon Hospital
Drayton High Road Norwich
NR6 5BE
Telephone: 01603 421120
Principal Professional Advisers
Bankers:
Barclays Bank plc
P.O. Box 885
Mortlock House Histon Cambridge CB24 9DE
Independent Examiner:
Helen Rumsey
Ensors Accountants LLP Connexions
159 Princes Street Ipswich
Suffolk IP1 1QJ
Report of the Corporate Trustee
The Corporate Trustee submits its Annual Report on the affairs of the Charity, together with the financial statements and independent examiner's report for the year ended 31 March 2023. The financial statements have been prepared in accordance with the accounting policies set out on pages 16-17, and comply with the Charitable Fund’s trust deed, the Charities Act 2011 and Accounting and Reporting by Charities: Statement of Recommended Practice applicable to charities preparing accounts in accordance with the Financial Reporting Standard applicable in the UK and Republic of Ireland (FRS 102).
Charitable Objectives
The Charity is an NHS umbrella charity registered with the Charity Commissioners for England and Wales. The objectives of the umbrella charity are for the Trustee to apply the income, and at their discretion, so far as may be permissible, the capital for any charitable purpose or purposes relating to the services provided by:
-
Norfolk and Suffolk NHS Foundation Trust
The funds are used to meet the objectives of the original donations or bequests, so far as is reasonably practicable. Where there are no specific objectives, the funds are used by the Charity for such purposes relating to services provided by them under the National Health Service Act 1977. The Charity meets the legal requirement of applying the funds for public benefit by ensuring that they are spent on the Trust’s service users and the staff who care for them.
Specific Restrictions
The funds are managed in accordance with the conditions set out in the Trustee Investments Act 1961 and the governing document.
All the Charity’s funds are regarded as designated funds for general purposes to particular NHS organisations or locations and are accounted for in accordance with the latest Guidance for NHS Charities from the Charity Commission. Twenty-eight funds are accounted for as unrestricted funds where the donor has made known their non-binding wishes to a particular area. The Trustee has adopted a policy of designating funds within the unrestricted funds in order to respect the wishes of our generous donors wherever possible.
Two funds are accounted for as restricted funds.
Structure, Governance and Management
The Charitable Funds Committee is a formal non-executive committee of the Trust’s Board of Directors and has no executive powers, other than those specifically delegated to it in its Terms of Reference.
The Charitable Funds Committee, a committee of the Corporate Trustee, met twice during the year and makes recommendations to the Corporate Trustee on:
-
Fund governance
-
Investment policies
-
Fundraising
-
Expenditure policies and procedures, and
-
Reporting arrangements
Designated Directors and Managers manage the funds within the umbrella Charity on behalf of the Corporate Trustee.
The funds are overseen by fund holders who can make recommendations on how to spend the money within their area. These recommendations are generally accepted, provided they meet a charitable principle and also correspond to the criteria of the purpose of the fund.
The accounting records and day to day administration of the funds are dealt with by the Assistant Financial Accountant, Endeavour House, Russell Road, Ipswich IP1 2BX.
The registered office of the Charitable Fund is:
Norfolk and Suffolk NHS Foundation Trust, Hellesdon Hospital,
Drayton High Road, Norwich
NR6 5BE.
Future Plans
The trustee does not expect any significant changes in the objectives of the Charity in the forthcoming year and will continue to receive and expend funds for the benefit of the Trust and its service users, and to support staff and service development where other sources are unavailable.
Principal Activities
Activities and achievements for public benefit
During the year the funds continued to support a wide range of charitable and health related activities benefiting both service users and staff.
In doing so the Trustees have had regard to the Charity Commission's guidance on public benefit and in general they are used to purchase additional equipment and services that the NHS is unable to provide from other sources.
There are three principal areas of activity within the Charity:
-
Contributions to the NHS – where funds are received and expended for the benefit of the NHS
There were no contributions to the NHS received or expended during 2022/23 (2021/22, Nil).
-
Patients’ welfare and amenities – where funds are received and expended for the benefit of service users.
Total expenditure for the year under this activity was £39,400 (2021/22, £50,100) of which the main expenditure is summarised below:
Expenditure included £11,900 from the Captain Sir Tom fund which was received and used for enhancing the well-being of service users impacted by COVID-19. Included in this were various garden projects which benefited from new fencing, plants and garden works totalling
£4,600 as well as a mix of sensory/ therapeutic items. The Sensory Room within Lark Ward was completed with a contribution from the Captain Sir Tom fund of £6,900.
Additional funding for the Sensory Room at Lark Ward of £10,500 came from the Suffolk East General Mental Health fund.
The Family Psychiatry fund used £1,500 to purchase copies of ‘The Happiness Trapp’ for the benefit of service users.
A total of £4,800 was spent by the Central Cluster Old People’s Legacy fund for numerous activities and equipment including outings, takeaways and afternoon tea, music equipment and kitchen/ gardening items.
The therapeutic garden at the Wedgwood Unit utilised £1,300 of the donations received specifically for this purpose, for designs and technical drawings.
Another £8,100 was spent on Christmas presents and festivities for the service users on the wards.
The remaining expenditure was given for smaller requests for the benefit of service users to enhance their experience
-
Staff welfare and amenities – where funds are received and expended for the benefit of staff
Expenditure for the year under this activity amounted to £15,400 (2021/22, £24,400)
of which the main expenditure is summarised below:
Expenditure included £4,100 received and used from the Captain Sir Tom fund for enhancing the well-being of NHS Staff and volunteers impacted by COVID-19. This funding provided a secure bike shed for staff at the Woodlands.
Black History Month celebrations totalling £4,700 were funded by the Trust Staff General fund. This was an opportunity for staff and service users to reflect and celebrate the events of the year.
Other expenditure included £1,500 for staff training in Interpersonal Therapy for Adolescents. This is aimed at the CFYP under 18’s Wellbeing service and will benefit the young people who use this service.
A further £3,900 funded specialist
support for the Communications team in co- production of literature and communications which ensured accessibility of such to the widest groups of people.
The remaining expenditure was given for smaller requests for the benefit of staff to enhance their experience.
Grant Making Policy
The Charity awards grants on an informal basis and in accordance with the objectives of the individual funds. The needs of the relevant hospital departments are considered, and grants are awarded in the circumstances where the NHS would not normally provide the equipment or service, and where there is a benefit to service users in the provision of the equipment or service. A Charitable Fund request form is completed in the first instance and is considered on its own merits with regard to service user needs and provision of sufficient public benefit.
Fund holders are entrusted with making decisions on grant making and will decide the appropriateness of each application. The Charitable Funds Committee monitors income and grant making during the financial year.
Fund holders are able to authorise grants up to £1,000. Approval from Service Directors is required for requests between
£1,000 and £5,000. The Chief Finance Officer is required to approve requests between £5,000 and £25,000. Applications between £25,000 and £100,000 need to be approved by the Charitable Funds Committee with anything over £100,000 requiring Board approval.
The Charity also occasionally accepts grants from other charities for the benefit of service users and transmits the donation on their behalf ensuring that the request of the donor is honoured. No donations of this type were received in the year. (2021/22, Nil).
Financial Review
As shown in the following Statement of Financial Activities, the total value of funds held by the Charity decreased from
£391,000 to £375,000. A total of £38,500 was given to the Charity in the form of donations and legacies. This was £13,200 more than last year. The Charity has not made any further investments in 2022/23 due to the lack of return and the need for
available cash to discharge grants.
Expenditure has reduced by £19,700 to £54,800. The independent examination fee for the year was £2,190.
The Charity encourages fund-raising by volunteers but does not depend on donations in kind to achieve its objectives.
The impact of the COVID-19 pandemic and the restrictions in place during 21/22 finally began to disappear throughout the Trust during 22/23 although events held were still minimal.
Donations from the public via the online community have continued to decrease but we have been very grateful to have received over
£1,600 in this way during 22/23 (2021/22,
£3,000).
The majority of the donations in 22/23 have been received for the benefit of the Wedgwood Therapeutic Garden with a total of £21,600 received. The garden once complete will help service user recovery by the practical, social and therapeutic elements of gardening, with the opportunity of building confidence and skills to keep people out of hospital.
The Trust is confident that there will be no further material financial impact on its activities as we enter a new financial year.
Reserves Policy
The Charity has been mindful of the need to reduce the level of reserves held and the Trustees will continue to review the balances held in the designated funds and encourage an appropriate level of expenditure. There are no target reserves as it is not the policy of the charitable fund to hold reserves. The fund holders are encouraged to spend monies on good causes rather than allowing funds to accumulate. The Charitable Funds Committee monitor any requests over £25,000 thereby anticipating the need to withdraw any investments that may be needed to fund approved grants.
Risk Management
Major risks to which the Charity is exposed have been identified and procedures have been put in place to mitigate those risks. All funds are checked and an assessment is undertaken before a payment is made to ensure that there is money available to meet expenditure.
Procedures are in place to safeguard the receipting of donations and the banking of cash and cheques. The Charitable Funds Committee monitors income and expenditure during the financial year. The Trustees have taken a cautious approach to investment by ensuring that assets are invested in low-risk ethical funds
and kept as cash holdings. Cash holdings that are set aside for day-to-day transactions are kept to a minimum.
Investment Policy
It is the policy of the Charity to ensure:
-
Effective and secure investment of charitable monies
-
Maximisation of investment income, and
-
Maintenance of appropriate working cash balances for day-to-day transactions
No investments were held within this current year due to poor interest return.
Going concern
The charity has no current liabilities and there are sufficient cash reserves. As a result, the trustees are confident that the charity is still considered to be a going concern.
In addition, the NHS Foundation Trust’s accounts for the 22/23 financial year have been prepared on a going concern basis; the independent auditor’s report has concluded that this is appropriate.
Statement of Trustee responsibilities in respect of the Trustee Annual Report and the financial statements
Under charity law, the Trustees are responsible for preparing the Trustee Annual Report and the financial statements for each financial year, which show a true and fair view of the state of affairs of the Charity and its incoming resources and application of resources for that year.
In preparing these financial statements, generally accepted accounting practice entails that the Trustees:
-
Select suitable accounting policies and then apply them consistently
-
Make judgements and estimates that are reasonable and prudent
-
State whether the recommendations of the Statement of Recommended Practice have been followed, subject to any material departures disclosed and explained in the financial statements
-
State whether the financial statements comply with the Trust deed and rules, subject to any material departures disclosed and explained in the financial statements
-
Prepare the financial statements on a going concern basis unless it is inappropriate to presume that the Charity will continue its activities
The Trustees are required to act in accordance with the Trust deed and the rules of the Charity, within the framework of trust law. They are responsible for keeping proper accounting records, sufficient to disclose at any time, with reasonable accuracy, the financial position of the Charity at that time, and to enable the Trustees to ensure that, where any statements of accounts are prepared by them under section 132(1) of the Charities Act 2011,
those statements of accounts comply with the requirements of regulations under that provision. They have general responsibility for taking such steps as are reasonably open to them to safeguard the assets of the Charity and to prevent and detect fraud and other irregularities.
Thank You
On behalf of the staff and service users who have benefited from the donations and legacies given, the Corporate Trustee would like to thank all service users, relatives, staff, and the general public for their generosity.
Further information:
If you require further information about the work and operation of the Fund, please contact the Chief Finance Officer, Norfolk and Suffolk NHS Foundation Trust, Hellesdon Hospital, Drayton High Road, Norwich, Norfolk NR6 5BE.
By order of the Trustee Signed:
Zoe Billingham
Chair
Date: 23rd November 2023
Jason Hollidge
Chief Finance Officer and Trustee Date: 23rd November 2023
Independent examiner’s report to the trustee of Norfolk and Suffolk NHS Foundation Trust Charitable Fund and Other Related Charities
I report to the trustee on my examination of the accounts of the Norfolk and Suffolk NHS Foundation Trust Charitable Fund and Other Related Charities (the Charity) for the year ended 31 March 2023.
Responsibilities and basis of report
As the trustee of the Charity you are responsible for the preparation of the accounts in accordance with the requirements of the Charities Act 2011 (‘the Act’).
I report in respect of my examination of the Charity’s accounts carried out under section 145 of the 2011 Act and in carrying out my examination I have followed all the applicable Directions given by the Charity Commission under section 145(5)(b) of the Act.
Independent examiner’s statement
I have completed my examination. I confirm that no material matters have come to my attention in connection with the examination giving me cause to believe that in any material respect:
-
accounting records were not kept in respect of the Charity as required by section 130 of the Act; or
-
the accounts do not accord with those records; or
-
the accounts do not comply with the applicable requirements concerning the form and content of accounts set out in the Charities (Accounts and Reports) Regulations 2008 other than any requirement that the accounts give a ‘true and fair view which is not a matter considered as part of an independent examination.
I have no concerns and have come across no other matters in connection with the examination to which attention should be drawn in this report in order to enable a proper understanding of the accounts to be reached.
Signed:
Mrs H Rumsey FCA Ensors Accountants LLP Connexions
159 Princes Street Ipswich
IP1 1QJ
Date:
Annual accounts
for the year ended 31 March 2023
Statement of Financial Activities
for the year ended 31 March 2023
| 2022/23 | 2021/22 | |||||
|---|---|---|---|---|---|---|
Unrestricted Funds | Restricted Funds | Endowment Funds | Total Funds | Total Funds | ||
Notes | £'000 | £'000 | £'000 | £'000 | £'000 | |
Income from | ||||||
Donations and legacies | 2 | 39 | - | - | 39 | 25 |
Total income | 39 | - | - | 39 | 25 |
|
Expenditure on |
||||||
|---|---|---|---|---|---|---|
Charitable Activities | 3 | (39) | (16) | - | (55) | (74) |
Total expenditure | (39) | (16) | - | (55) | (74) |
Net (expenditure) / income
Transfer of funds
Net movement in funds
Fund balances brought forward at 1 April 2022
Fund balances carried forward at 31 March 2023
All income and expenditure is derived from continuing activities.
All gains and losses recognised in the year are included in the Statement of Financial Activities. The notes on pages 16 to 25 form part of these accounts.
Balance sheet
as at 31 March 2023
Total Total
Unrestricted Restricted Endowment
Funds Funds Funds 31-Mar-23 31-Mar-22
|
Notes |
£'000 | £'000 | £'000 | £'000 | £'000 |
|---|---|---|---|---|---|
Current Assets Cash at bank and in hand | 309 | 66 | - | 375 | 391 |
Current Assets | 309 | 66 | - | 375 | 391 |
Total Assets | 309 | 66 | - | 375 | 391 |
Liabilities
Current Liabilities - - - - -
Total Assets Less Current Liabilities
309 66 - 375 391
Funds of the Charity
Unrestricted/Restricted:
7
309 66 -
The notes on pages 16 to 25 form part of these accounts.
These financial statements were approved by the Corporate Trustee and signed on its behalf by
Jason Hollidge
Chief Finance Officer and Trustee Date: 23rd November 2023
Statement of cash flows
for the year ended 31 March 2023
| Note | Total | Total | |
|---|---|---|---|
31-Mar 2023 | 31-Mar 2022 | ||
| £'000 | £'000 | ||
Cash Flows from operating activities: | |||
Net cash from activities 9 | (16) | (49) | |
Cash flows from investing activities: Proceeds from sale of investments | - | - | |
Net cash provided by investing activities | - | - | |
Cash in change and cash equivalents in the reporting period | |||
Cash and cash equivalents at the beginning of the reporting period | 8 | 391 | 440 |
Change in cash and cash equivalents in the reporting period | (16) | (49) | |
Cash and cash equivalents at the end of the reporting period | 8 | 375 | 391 |
Notes forming part of the financial statements
-
Accounting Policies
-
Basis of preparation and assessment of going concern
-
The financial statements have been prepared in accordance with the accruals concept and have been prepared under the historical cost convention.
The financial statements are prepared in sterling, which is the functional currency of the Charity. Monetary amounts in these financial statements are rounded to the nearest thousand £.
The financial statements have been prepared in accordance with the Charity’s governing document, the Charities Act 2011 and “Accounting and Reporting by Charities: Statement of Recommended Practice applicable to charities preparing their accounts in accordance with the Financial Reporting Standard applicable in the UK and Republic of Ireland (FRS 102)” (as amended for accounting periods commencing from 1 January 2019).
The financial statements are prepared on a going concern basis and the principal accounting policies have been applied consistently throughout the year. The trustees consider that there are no material uncertainties about the charity's ability to continue as a going concern.
The Charity constitutes a public benefit entity as defined by FRS 102.
The accounts have departed from the Charities (Accounts and Reports) Regulations 2008 only to the extent required to provide a true and fair view. This departure has involved following the Statement of Recommended Practice for charities applying FRS 102 rather than the version of the Statement of Recommended Practice which is referred to in the Regulations, but which has since been withdrawn.
-
Critical accounting estimates and judgements
In the application of the charity's accounting policies, the Trustees are required to make judgements, estimates and assumptions about the carrying amount of assets and liabilities that are not readily apparent from other sources.
The estimates and associated assumptions are based on historical experience and other factors that are considered to be relevant.
Actual results may differ from these estimates.
The estimates and underlying assumptions are reviewed on an ongoing basis. Revisions to accounting estimates are recognised in the period in which the estimate is revised where the revision affects only that period, or in the period of the revision and future periods where the revision affects both current and future periods.
-
Financial Instruments
The Charity has elected to apply the provisions of Section 11 'Basic Financial Instruments' and Section 12 ' Other Financial Instruments Issues' of FRS 102 to all of its financial instruments.
Financial instruments are recognised in the Charity's balance sheet when the Charity becomes party to the contractual provisions of the instrument.
Financial assets and liabilities are offset, with the net amounts presented in the financial statements, when there is a legally enforceable right to set off the recognised amounts and there is an intention to settle on a net basis or to realise the asset and settle the liability simultaneously.
Basic financial assets
Basic financial assets, which include debtors and cash and bank balances, are initially measured at transaction price including transaction costs and are subsequently carried at amortised cost using the effective interest method unless the arrangement constitutes a financing transaction, where the transaction
is measured at the present value of the future receipts discounted at a market rate of interest. Financial assets classified as receivable within one year are not amortised.
Basic financial liabilities
Basic financial liabilities, including creditors are initially recognised at transaction price unless the arrangement constitutes a financing transaction, where the debt instrument is measured at the present value of the future payments discounted at a market rate of interest. Financial liabilities classified as payable within one year are not amortised. Debt instruments are subsequently carried at amortised cost, using the effective interest rate method.
Derecognition of financial liabilities
Financial liabilities are derecognised when the Charity's contractual obligations expire or are discharged or cancelled.
-
Fund Accounting
The Charity maintains a general unrestricted fund which represents funds which are expendable at the discretion of the Trustees in furtherance of the objects of the Charity. Such funds may be held in order to finance both working capital and capital investment.
Restricted funds are provided to the Charity for particular purposes, and it is the policy of the Board of Trustees to carefully monitor the application of those funds in accordance with the restrictions placed upon them.
Endowment funds are subject to specific conditions by donors that the capital must be maintained by the Charity.
-
Income
-
Income is generated from voluntary donations, legacies, fundraising events and interest on cash at bank. The charity does not undertake charitable trading.
-
All income is included in full in the Statement of Financial Activities as soon as the following three factors can be met:
-
Entitlement - control over the right or other access to the economic benefit has passed to the charity
-
Probable - where it is more likely than not that the economic benefits associated with the transaction or gift will flow to the charity
-
Measurement - the monetary value or amount of the income can be measured reliably and the costs incurred for the transaction and the costs to complete the transaction can be measured reliably
-
-
Legacies
-
-
Legacies are accounted for as incoming resources either upon receipt or where the receipt of the legacy is probable.
This will be once confirmation has been received from the representatives of the estate that probate has been granted, the executors have established that there are sufficient assets in the estate to pay the legacy and all conditions attached to the legacy have been fulfilled or are within the charity's control.
If there is uncertainty as to the amount of the legacy and it cannot be reliably estimated then the legacy is shown as a contingent asset until all of the conditions for income recognition are met.
-
Investment income
The Trust implements a charitable funds investment policy to ensure:
-
Effective and secure investment of charitable monies
-
Maximisation of investment income
-
Maintenance of appropriate cash balances for day-to-day transactions
There was no investment income received during this current year.
-
Expenditure
The corporate trustee recognises liabilities in the accounts once they have incurred either a legal or constructive obligation to expend funds.
Expenditure for patient welfare, staff welfare and other contributions to the NHS are included in Charitable Activities. Expenditure is incurred directly by the charity in support of the NHS and is allocated to the appropriate fund.
Expenditure was incurred as follows:
| Total | Total | |
|---|---|---|
| 31 March | 31 March | |
| 2023 | 2022 | |
Unrestricted | £'000 | £'000 |
Other patients' | ||
welfare and amenities | 28 | 19 |
Other staff welfare
At any one-time Norfolk and Suffolk NHS Foundation Trust holds balances for debtors and creditors relating to the transactions it processes on behalf of the Charity, which are normally settled within the following month.
-
Grants made to institutions
Grants are made in furtherance of the charitable objectives of the fund in accordance with the governing document which established the charity for purposes relating to the NHS.
During the year no grants were paid (2021-22, Nil).
-
Grants paid to individuals
During the year the charity made no small grants relating to patients’ welfare (2021-22, Nil).
and amenities
11 1
39 20
-
Summary andstructure of funds
Restricted £'000 £'000 Other patients'
The report of the corporate trustee describes the structure of the funds. A summary of the
welfare and
amenities
Other staff welfare and amenities
12 31
4 23
16 54
funds as at 31 March 2023 is given below. The charity adheres to a policy that no transfers are made between funds unless in exceptional circumstances, for example where a fund is being wound up and the remaining balance is transferred to a comparable fund.
The 30 funds held by the Charity fall under the management of Norfolk and Suffolk NHS Foundation Trust. Charges for the annual Independent Examination and administration fees are therefore met by Norfolk and Suffolk NHS Foundation Trust. The independent examination fee for the year was £2,190 (2021-22,
£1,995).
-
Related party transactions
During the year none of the members of the key management staff or parties related to them have undertaken any material transactions or received any remuneration or expenses from the charitable fund (2021-22, Nil).
The charitable trust has made no revenue or capital payments to Norfolk and Suffolk NHS Foundation Trust. There were no outstanding balances at year end.
If no restriction is conveyed by the donor, funds are placed in the designated area that the donation is gifted.
No endowment funds were held during the current year.
Unrestricted Funds
Norfolk and Suffolk NHS FT
Balance Income Expenditure Transfers
Gains
Balance
of Fund
Foxhall House LSU
Wedgwood Patients
Central Cluster Older
Chatterton House
Gt Yarmouth
Trust Wide
West Norfolk
Suffolk East General Mental Health
Young Carers
Others (18 funds) Total
benefit of the Insight Magazine
General Purpose fund designated for the benefit of service users at the LSU (Low Secure Unit)
General purpose fund designated for Wedgwood patients
General purpose fund designated for older people and dementia
General Purpose fund designated for Chatterton House
General Purpose fund designated for Great Yarmouth Services
General purpose fund designated for Trust Wide services General purpose fund designated for services in West Norfolk
General purpose fund designated for the benefit of service users in the Suffolk East Location
General Purpose fund designated to benefit Young Carers in the community
Restricted Funds
Norfolk and Suffolk NHS FT
-
Restricted Funds:
Balance Income Expenditure Transfers 1 April
2022
Gains and Losses
Balance 31 March
2023
of Fund
The Lanes
volunteers and service users
Fund designated to benefit the Dialectical Behaviour Therapy programme
- - - - - -
Total 82 - (16) - - 66
Unrestricted Funds
Norfolk and Suffolk NHS FT
-
Unrestricted Funds:
Balance Income Expenditure Transfers 1 April
2021
Gains and Losses
Balance 31 March
2022
of Fund
Foxhall House LSU
Wedgwood Patients
Central Cluster Older
Chatterton House
Gt Yarmouth
Trust Wide
West Norfolk
Suffolk East General Mental Health
Young Carers
benefit of the Insight Magazine
General Purpose fund designated for the benefit of service users at the LSU (Low Secure Unit)
General purpose fund designated for Wedgwood patients
General purpose fund designated for older people and dementia
General Purpose fund designated for Chatterton House
General Purpose fund designated for Great Yarmouth Services
General purpose fund designated for Trust Wide services
General purpose fund designated for services in West Norfolk
General purpose fund designated for the benefit of service users in the Suffolk East Location
General Purpose fund designated to benefit Young Carers in the community
Others (16 funds) 57 5 - - 62
Total 319 10 (20) - - 309
Norfolk and Suffolk NHS Foundation Trust Charitable Funds Annual Report 1st April 2022 to 31 s t March 2023 21
-
Summary and Structure of Funds (continued)
| Material Funds Restricted | ||||
|---|---|---|---|---|
Norfolk and Suffolk NHS FT | Balance | Income Expenditure Transfers | Gains | Balance |
- Restricted Funds: | 1 April 2021 | and Losses | 31 March 2022 |
Material Funds
Captain Sir Tom
The Lanes
Na of Fu be
volunteers and service users
Fund designated to benefit the Dialectical Behaviour Therapy
- 15 (15) - - -
programme Total 121 15 (54) - - 82
Summary
| Total | Total | |
|---|---|---|
|
31 March 2023 £'000 |
31 March 2022 £'000 |
|
Endowment funds | - | - |
Restricted Funds | 66 | 82 |
Unrestricted Funds | 309 | 309 |
Total Funds | 375 | 391 |
Funds have arisen from a variety of sources principally legacies and donations
-
Analysis of Net Assets between funds
|
Unrestricted Funds £'000 |
Restricted Funds £'000 |
Endowment Funds £'000 |
Total 31 March 2023 £'000 |
Total 31 March 2022 £'000 |
|
|---|---|---|---|---|---|
Current assets - Cash at bank and | 309 | 66 | - | 375 | 391 |
in hand | |||||
| 309 | 66 | - | 375 | 391 |
|
Unrestricted Funds £'000 |
Restricted Funds £'000 |
Endowment Funds £'000 |
Total 31 March 2022 £'000 |
Total 31 March 2021 £'000 |
|
|---|---|---|---|---|---|
Current assets - Cash at bank and | 309 | 82 | - | 391 | 440 |
in hand | |||||
| 309 | 82 | - | 391 | 440 |
Analysis of Cash and cash equivalents
| Total | Total | |
|---|---|---|
|
31 March 2023 |
31 March 2022 |
|
| £'000 | £'000 | |
Cash in hand | 375 | 391 |
Total cash and | 375 | 391 |
cash equivalents
Cash and cash equivalents
Cash and cash equivalents include cash in hand, deposits held at call with banks, other short- term liquid investments with original maturities of three months or less, and bank overdrafts.
Reconciliation of net income / (expenditure) to net cash flow from operating activities
| Current Year | Prior Year | |
|---|---|---|
| £'000 | £'000 | |
Net (expenditure) / income for the reporting | ||
period (as per the statement of financial activities) | (16) | (49) |
Adjustments for: Decrease in debtors | - | - |
(Decrease) in creditors | - | - |
Net cash (used in) / from operating activities | (16) | (49) |
| 2021/22 | |||||
|---|---|---|---|---|---|
Unrestricted Funds | Restricted Funds | Endowment Funds | Total Funds | ||
| Notes | £'000 | £'000 | £'000 | £'000 | |
Income from | |||||
Donations and legacies | 2 | 10 | 15 | - | 25 |
Total income | 10 | 15 | - | 25 |
|
Expenditure on |
|||||
|---|---|---|---|---|---|
Charitable Activities | 3 | (20) | (54) | - | (74) |
Total expenditure | (20) | (54) | - | (74) |
|
Net (expenditure) / income |
(10) | (39) |
- (49) |
|
|---|---|---|---|---|
Transfer of funds | - | - | - - | |
Net movement in funds | (10) | (39) | - (49) | |
Fund balances brought forward at 1 April 2021 | 319 | 121 | - | 440 |
Fund balances carried forward at 31 March 2022 | 309 | 82 | - | 391 |














Trust Headquarters:
Hellesdon Hospital Drayton High Road Norwich
NR6 5BE
 01603 421421
01603 421421

 nsft.nhs.uk
nsft.nhs.uk @NSFTtweets NSFTrust
@NSFTtweets NSFTrust
Norfolk and Suffolk NHS Foundation Trust values and celebrates the diversity of all the communities we serve. We are fully committed to ensuring that all people have equality of opportunity to access our service, irrespective of their age, gender, ethnicity, race, disability, religion or belief, sexual orientation, marital or civil partnership or social and economic status.

Change and improvement update – November 2023
1. Executive summary
The newly established Change and Improvement team has three immediate priorities:
Establishing the Change Portfolio for the organisation
The Trust has established a Change Portfolio for the organisation. The aim of the Change Portfolio is to provide oversight of all the major change within the Trust. This oversight will allow control and prioritisation of major change, driven by the Trust strategy and annual planning cycles.
An established change delivery framework
A toolkit is being developed to deliver change through consistent products and processes. Alignment to the Trust Quality Improvement (QI) approach. Refresh of business case and impact assessment processes.
With the support of NHSE, commencement of a regular assessment of organisational improvement capability. Helping to identify areas for development and improvement around the change journey.
Building high performing change resource
The Change and Improvement team has successfully recruited to several internal posts to help sustain long term improvement within the Trust. A staff survey is being developed to inform the needs and expectations of the change community across the organisation.
Improving together - Inspirational People | Exceptional Care | Transforming Lives
1. Executive summary (2)
Oversight of the change portfolio enables the Trust to co-ordinate activity on Improvement Priorities:
Trust Strategies and Annual Planning
Launch of the Trust strategy and development of key sub-strategies. Enabling an informed annual planning cycle from 2024/25 onwards. Building on key stakeholder relationships with stakeholders, including major collaboratives across both counties and regionally.
Financial Performance linked to delivery of change
A combined focus on quality and financial improvement. Oversight of efficiency and value improvement deliverables, alongside capital plans and financial recovery initiatives.
Improvement Programme and Recovery Support Programme (RSP)
Co-ordination of improvement pillars with wider organizational change programmes. Identifying opportunities for efficiency and common deliverables and benefits.
Trustwide enablers
Large scale change that enables service improvements and better outcomes for service users, carers and staff. Including major estates and digital programmes and projects, alongside re-tendering for existing services or securing new funding opportunities.
Improving together - Inspirational People | Exceptional Care | Transforming Lives
Improvement Programme update – November 2023
1. Our phased programme to deliver sustained improvement
PHASE 1
Insight and acknowledgement, performance recovery
Our history as a Trust, of our real challenges, of improvement, of excellent practice not consistently maintained
April 2022
Root cause diagnostic with stakeholders of factors preventing sustained improvement
Trust-wide Improvement Programme with system partner support established
1st Big Conversation online engagement platform with over 5,000 staff (Q3 22/23), Culture programme launched
Feb 2023
PHASE 2
Consolidation and capability building
Recovery Support Programme planned exit, continued quality improvements, financial sustainability gains
Trust Strategy and Model of Care launched. Mental Health Collaboratives launched with ICBs (Q1 23/24)
Our Next Conversation online engagement platform with over 5,000 staff (Q1 23/24), Vision, purpose and values
CQC ‘Must Do’s’ reduced from 108 to 30. Section 29a lifted
PHASE 3
Transformation and innovation
Continuous improvement method, positive culture change, clinical excellence and innovation
Greater collaboration, strengthening partnering at system, place and neighbourhood




Improving together - Inspirational People | Exceptional Care | Transforming Lives
Phase 2 of our Improvement Programme commenced in March 2023 following the improved CQC report received in February 2023. We continue to progress against key delivery milestones across all areas.
Improvements made
Governance:
-
In November 2023, an internal audit review of the Improvement Programme and progress to exiting Recovery Support Programme 4. The review looked to ensure the programme to delivery exit from NHSEI’s RSP Level 4 is robustly governed and on track to deliver. The review looked to ensure that all completed action is supported by evidence of delivery. It reached a conclusion of ‘Substantial Assurance’, the highest available rating, validating our position.
-
The Recovery Support Programme (RSP) Review Group continuous to meet monthly. This group is chaired by a NED, and reviews evidence relating to our RSP criteria, recommending sign off to our NHSE regional team.
Improvement pillars:
Our four pillars are supporting delivery of the Strategic Initiatives we set out in our strategy and are addressing the root cause challenges faced by the Trust. Key activities include:
-
Culture and Leadership: Culture dashboard established with culture strategy draft to be completed in November for sign off in January. Recruitment and retention plan developed, with fair recruitment panels established.
-
Quality and Safety: Early Warning Trigger Tool (MEG) implementation to be completed for planned teams to provide oversight and assurance of all clinical audits, with immediate outcomes available for review.
-
Access, Data and Delivery: IQPR report established, integrated into QPM meetings, with Power BI dashboard now in development to improve functionality.
-
Model of Care: MoC developed, with MoC recovery plan and revised timeline developed. Global Assessment Framework (GAF) pilots have been completed, with the GAF now being rolled-out more widely. Treatment pathway mapping in progress to assess our pathway against best practice.
Measuring impact
Outcomes Dashboard: We have developed an outcomes dashboard to track the impact and improved outcomes that we are aiming to deliver through Phase 2 of the Improvement Programme. This is reviewed at Exec and SLT, as well as Improvement Board and Audit and Risk Committee. We now have plans to develop the dashboard further to ensure that we collect data in a more timely way (where available), with outcomes reporting built into regular workstream and pillar reporting. Improving together - Inspirational People | Exceptional Care | Transforming Lives
Evidencing progress
CQC Must Do delivery:
-
We continue to deliver our CQC Must Dos through local action plans. Actions are reviewed and signed off at the Evidence Assurance Group, a multistakeholder panel chaired by Frankie Swords the N&W ICS Medical Director with representation from partners and patient representative groups.
-
29% of our Must Dos have been signed off with an agreed trajectory to review and sign off the remainder of our Must Dos between December 2023 and March 2024, completing all Must Dos within the financial year as per our plan.
RSP Exit Criteria:
-
We continue to deliver the agreed RSP criteria, as shown by the detailed RSP Plan on a Page.
-
50% of our RSP criteria has formally been approved by the NHS England regional team as complete
-
Due to the arrival of our new trust CEO and a new NSHE Improvement Director, we are reviewing some items which will likely result in a short delay to their delivery. This is being discussed and supported by the NHS England regional team.
-
Those items under review and likely to be delayed into 2024 are:
-
1.1 – Trust Strategy and sub-strategies: Review of the sub-strategies timeline to ensure sufficient people participation and service user engagement
-
1.2 – Operational Restructure: The overall timeline for completion of the restructure is under review from the incoming CEO and will likely move into early 2024. This delay will have a knock-on impact on evidence relating to the restructure.
-
2.2 – Learning from Deaths: In light of the recent mortality review, we need to review and strengthen the evidence to be brought to fulfil theme 2.2 and agree with partners what they would need to see to be assured of completion.
-
3.1 – Board Membership: In response to recent changes in the NSFT Executive Team, we are reviewing the evidence for this theme
-
-
Monthly RSP meetings are planned for the remainder of the financial year to review and sign off the remainder of the criteria
Risks
The following represent the key risks to the Improvement programme:
|
Risk |
Mitigation |
|---|---|
If we do not strike the balance between continued improvement, and sustaining the improvements already delivered, we risk eroding improvements already made. |
|
If programme and quality governance mechanisms do not identify risks early, we cannot address them before they become more significant risks or issues |
|
Phase 2 – plan on a page linked to our Trust strategic objectives
APR MAY JUN JUL AUG SEP OCT NOV DEC JAN FEB MAR
CULTURE AND LEADERSHIP
Next Conversation launch
Culture dashboard developed
Staff survey promotion and
launch
Final draft culture strategy
Culture strategy sign off
Staff experience a just and open culture and are motivated to work for NSFT.
Leadership Competency
Framework developed
Ongoing delivery of Leading Confidently / Senior Leader programmes
Recruitment and retention plan developed
Exit interview policy and processes
reviewed and enhanced
Exit interview responses processes enhanced
Improved pathway of students into posts
MODEL OF CARE
A defined way to provide care, treatment, organise services and use resources.
Draft ready for review
Model of Care and Model of Care + aligned
Model of Care final draft Implementation plan and resources agreed Implementation of Model of Care as per Implementation Plan
ACCESS, DEMAND AND DATA
Equitable access to services, with data used to match capacity with demand.
QUALITY AND SAFETY
Improved and consistent quality of care provided to our service users.
Stable IQPR report developed
Pharmacy culture programme delivered
Improve consistency of QPM meeting packs
Integrate Power BI reporting into Care Group reporting Delivery against recovery trajectories
Medicines Management Policy developed (delayed to end of November)
Physical Health Competency Framework launched
IQPR data warehouse and Power BI reporting developed and stable
Medicines Optimisation Strategy developed and aligned with MoC
CQC MUST Dos
Plan to address 30 Must Dos submitted to CQC
Early warning trigger tool rolled out to Adult Acute
and Community, Older Peoples and CRHT Teams
Delivery against remaining Must Dos, with EAG assurance process
Quality and safety issues to address
RSP EXIT CRITERIA
MDs reviewed at June
EAG
RSPG
MDs reviewed
at Aug EAG
Delivery of RSP criteria
MDs
reviewed
at Oct EAG
MDs
reviewed at Nov EAG
MDs reviewed
at Jan EAG
MD
reviewed
at Feb EAG
All MDs
reviewed
and signed off
RSG sign off
Deliverables to demonstrate
RSP criteria
review of
Monthly RSPG review of completed RSP criteria, reported into bi-monthly RSG meeting
of completed
organisational improvement
finalised with region
completed RSP criteria
RSG sign off of completed criteria
RSG sign off of completed criteria
RSG sign off of completed criteria
criteria
Improving together - Inspirational People | Exceptional Care | Transforming Lives
Key:
Ongoing activity Milestone Complete milestone RSP milestone RSP complete milestone
RSP exit criteria in detail
Key:
Measuring Impact - Improvement Programme Outcomes Dashboard
-
We have developed an Outcomes Dashboard for the Improvement Programme to track key metrics that will show whether our work is delivering, and sustaining, the positive impact planned.
-
We have published our second dashboard in November 2023, with updates to follow on a quarterly basis. As the second iteration of this dashboard, we have limited data points on which to base our analysis. This will continue to improve as the dashboard matures.
Improvement Programme Outcomes summary
-
The second iteration of the Improvement Outcomes dashboard suggests:
-
Culture and Leadership: Improvement in several aspects of our recruitment and retention position, improved BME representation and consistent improvement in the overall retention rate. The area of concern with regards to recruitment and retention is the steadily increasing rate of turnover for those who have been with the Trust for less than two years. This is the focus of our Recruitment and Retention Plan, with high impact actions agreed and administrative staff identified as a target group.
-
Quality and Safety: The dashboard shows mixed outcomes and compliance rates. Rollout of the Early Warning System is on track, with a consistently high uptake in the audit cycles across inpatient, community and crisis teams. However, overdue risks and incidents are not seeing the same levels of improvement. Work is being done within the pillar to further address this, including enhancements to the Trust approach to risk, and investigating blockers to the signing off incidents.
-
Access, Demand and Data: Referral to assessment and Waiting List data highlights the variation between Care Groups, with bespoke initiatives in place across different services. Referral to treatment data has shown overall improvement and a continued reduction in waiting times since peaking in March 2023.
-
Model of Care: The dashboard shows the results of the GAF pilot across three teams with 40 patients. The results were positive and showed that over the 6-week pilot, patients receiving treatment in a PICU, adult inpatient and adult community ward all saw significant health gains (measured by the difference in GAF scoring from the start of the pilot to the end).
-
Improving together - Inspirational People | Exceptional Care | Transforming Lives
Collaboratives update – November 2023
East of England Provider Collaborative
-
Two NSFT business cases approved – CAMHS Alternative to Admission Team (CATAT) and Community Forensic
-
Community Forensic – Developing stepped down services to locality services, including consultation and advice; case management; joint working and training to support discharge management; and intensive support to avoid admissions and reduce length of stay.
-
CATAT - to reduce admissions to Tier 4 beds by providing additional support at the point of admission.
-
Recurrent funding of £515k and £665k respectively
-
Provider Collaborative is in a robust financial position
-
NSFT to consider further opportunities to draw in funding linked to Provider Collaborative objectives of reducing out of area activity and in- patient activity through community transformation
Improving together - Inspirational People | Exceptional Care | Transforming Lives
-
Agreed to work towards one NSFT contract across Norfolk and Suffolk – NSFT, Norfolk & Waveney ICB, Suffolk & North East Essex ICB
-
The next stage is for contracts, quality, transformation task and finish groups to be set up to take forward agreed actions and for a second workshop to be held on Friday 24 November or Friday 1 December.
-
It was agreed that a joint meeting of all three organisations to focus on strategy and ways of working would take place with selected members of the Executive and Board to make the meeting manageable.
-
Aligns with NSFT Model of Care work
Improving together - Inspirational People | Exceptional Care | Transforming Lives
-
The Provider Selection Regime (PSR) will replace the existing procurement framework for arranging healthcare services in England – comes into force in Jan 2024
-
The aim of the PSR is to promote integration and enhance collaboration by providing a more flexible and proportionate process for commissioning healthcare services
-
The future arrangements will set out three separate provider selection processes by which commissioners can award contracts for relevant healthcare services:
-
Direct Award - Continuation of existing arrangements
-
The most suitable provider process This award process allows relevant authorities to make a judgement as to which provider is most suitable
-
The competitive process
-
Improving together - Inspirational People | Exceptional Care | Transforming Lives
-
Mental Health Collaborative Strategy/Outcomes Framework – To develop an outcomes framework based on Collaborative priorities
-
Talking Therapies - Satisfied with the performance and joint work of current provider, adopted Most Suitable Provider Option
-
Urgent & Emergency Care (UEC) - Partners are continuing to develop the UEC dashboard to track how investment in the system is making a difference to demand on services.
-
Mental Health Practitioners in Primary Care – For opted out PCNs proposal to collaborate much closer with Suffolk Integrated Neighbourhood Teams (INTs) and have the ambition to deliver the same service but outside of the GP practices.
Improving together - Inspirational People | Exceptional Care | Transforming Lives
Norfolk & Waveney Mental Health Collaborative
-
Dementia Charter - Proposed that all partners sign up to the Dementia Charter and commit to relevant deliverables. This would involve identifying a dementia lead for NSFT
-
Community Transformation - The aim of the stock take is to benchmark progress against the original proposal that secured Community Transformation funding. This would enable the current position to be understood and evaluated as preparation for the annual planning round for 2024/25
Improving together - Inspirational People | Exceptional Care | Transforming Lives
Public Accounts Committee – Progress in improving mental health services
-
Workforce shortages - Draft People and Culture Strategy sets out our approach to recruitment and retention. We will need to do more detailed work on details for specific groups of staff, but this should be part of an Integrated Care System (ICS) Workforce Strategy and we should/will raise with them.
-
Data and information for NHS mental health services still lags behind that for physical services. – Our Performance Team are doing a lot of work on data quality and is a key part of our improvement agenda.
-
New integrated care boards and partnerships could struggle to prioritise mental health services and support – We have got commitments from both of our Integrated Care Boards (ICBs) to maintain Mental Health Investment Standard spending and to mainstream after 3-year Community Transformation budget comes to an end in March 24.
-
The Department and NHS England have still not committed to rolling out waiting times standards to all mental health services. – As part of our work on Community Transformation we have set targets to reduce waiting times, reduce length of stay, reduce re-admissions, reduction in crisis presentations, increasing diagnosis rates, etc
-
Preventive and public health services for mental health have not had the same priority and focus on improvement as NHS mental health treatment services. – Part of Suffolk & Northeast Essex and Norfolk & Waveney ICB Groups that focus on healthy inequalities and prevention.
Improving together - Inspirational People | Exceptional Care | Transforming Lives
|
Report To: |
Board of Directors |
|---|---|
Meeting Date: | 23rd November 2023 |
Title of Report: | People and Culture Committee Chairs’ Reports |
Purpose of report: | For Assurance |
Authors: | Tricia Fuller, Non-Executive Director |
Director: | Zoe Billingham, Chairperson |
Link to Trust Strategy | Inspirational People; enabling our staff to thrive |
Legislation / compliance | CQC Well-Led; NHSE performance framework. Employment legislation |
Link to BAF / Risks | BAF risk 1.1 Failure to recruit and retain safe levels of high calibre staff and support positive values, culture and speaking up |
Executive Summary:
This report provides information, assurance and escalations from the meeting of the People and Culture Committee held on 9 November 2023.
Recommendation
The Board is asked to note the report.
People and Culture Committee Meeting – 9 November 2023
The Board is asked to note that the People and Remuneration Committee has been renamed and split into 2 committees (1) People and Culture and (2) Remuneration. This gives a clearer delineation between the remit of the committees.
Positive Assurances
The reduction in sickness absence continues and is now below target and that set by the ICB to be achieved by March 2024.
Staff turnover also continues to reduce, all areas apart from staff with under 2 years’ service are below target. Voluntary leavers are at 10.7%, a reduction of 4% in the last 12 months. Voluntary leavers for both medical and nursing staff have reduced to 4.8% and 8.9% respectively. Whilst the percentage of leavers with less than 2 years’ service remains high when taken as a percentage of total leavers, the actual numbers have reduced from 274 to 238. Whilst this is heading in the right direction there is still work to be done to reduce further.
The improvements in these two areas are not an overnight achievement but are the result of interventions and actions over a considerable period.
The number of calls to the FTSU Guardian have reduced with evidence of managers now proactively contacting the guardian for assistance to resolve issues. This committee will continue to monitor this and was pleased to note that the service has been extended by a further year.
The work on the Culture and Leadership pillar remains at a high standard and is on target.
The payroll Errors Group provided strong evidence that there are better controls in place with line of sight as to why errors on under/over payments are being made. 1% of errors (55 staff) identified where staff had been paid incorrectly or late. The committee were assured that where this happens staff will have their pay issue resolved in a timely manner. Late payments have been a long-standing issue in the Trust, and it is reassuring to see the improvement. Over payments however remain at an unacceptable level but with improved controls the expectation is that these should reduce. The committee will continue to monitor.
Areas of concern/Key Risks to Escalate
As notified to the Board in September compliance with undertaking appraisals, supervision and MAST is well below target and have fallen further, at the lowest level for a year. Work is underway to identify a dedicated resource to help to increase these levels. However, this is only a short-term solution to get to target. It’s important that we get to the root cause of this issue and that training development and leadership interventions are provided to ensure staff have the time to complete these sessions and that these are meaningful.
The committee expressed disappointment not to have had a Safer Staffing paper for a significant period and have asked for this to be reinstated. Work has been undertaken to ensure that there is line of sight as to where staffing challenges exist. It was agreed that Safer Staffing should also feature on the QAC agenda due to the impact on quality and safety.
The committee had a verbal update on Job Planning which is not effective with staff reporting issues with the Allocate system. Staff report job planning has been undertaken but not put on the system which doesn’t allow for auditing. Further work to be undertaken with a comprehensive report to the next committee.
The committee were also disappointed that the promise of admin support to clinical teams had not been achieved and have asked for a response at pace. Expecting clinicians to manage their own admin tasks greatly dilutes the time available to see patients, is not an effective use of a valuable resource and is demoralising for these staff.
These areas of concern are underpinned by a lack of accountability which needs addressing.
The committee noted that there will be a delay in finalizing the Reasonable Adjustment Policy and internal audit target will be missed by 6 months.
Major Actions/Commissioned Work Underway
Significant work has been undertaken on the BAF which has been streamlined and the committee now has just one BAF which allows for greater scrutiny. However, some of the controls and assurances need to be reviewed, further work to be undertaken.
Strategic Objective 1 – Inspirational People
Risk Description 1.1 Failure to recruit and retain safe levels of high calibre staff and support positive values, culture and speaking up. Risk Appetite – the Trust has very low/averse appetite for risks that impact on safe staffing, calibre of leadership, poor culture, and impact on ability of staff to speak up
Date last reviewed:
November 2023
Director Lead: Cath Byford, Chief People Officer and Deputy CEO
Board Committee:
People and Culture Committee
Consequence of risk:
If the trust fails to recruit and retain staff with the right values, skills and competencies and support the right culture then this impacts on delivering safe and effective services
Target Rating: (l x c) and Date to reach target
3 x 4 = 12 December 2025
Risk Rating over time
30
20
10
0
Rationale for current score: (l x c)
Metrics show performance in key areas not improving as yet, culture change is longer term. Review of workforce dashboard to prioritise focus and timescales
Jan-23 Mar-23 May-23 Jul-23 Sep-23 Nov-23
Controls (what are we currently doing about the risk?)
-
Improvement Programme culture and leadership pillar work
-
Safe staffing - e-rosters, safe staffing tool, nursing establishment review, agency cover for vacancies (with agency approval process); job planning
-
Recruitment & retention controls: Fair Recruitment panels; TRAC & Recruitment Pipeline Management & Recruitment Standards; values based recruitment; exit interviews and early conversations; Recruitment and retention group; medical recruitment strategy. New corporate and clinical induction; follow up of new staff. Absence management programme
-
Leadership controls: Leadership competency Framework; Leadership development programme; talent management programme, Board succession planning process; Board and senior leaders development;
-
Independent Freedom to Speak Up Guardian service
-
Big Conversation, quarterly pulse surveys, Staff survey, medical engagement survey
-
Care Group local governance committees and QPMs – scrutiny of key workforce metrics
-
System wide integrated workforce plan is aligned with corporate strategy
Assurances (how do we know if the things we are doing are having impact?)
-
Integrated Quality Performance Report (IQPR) workforce metrics, reported to People & Remuneration Committee and Board show: annualised sickness absence levels outside of target but reducing, supervision and appraisal remain below target; mandatory training improved with most care groups close to target; number of staff in post continues to increase, but medical vacancies remain an issue. Turnover of staff is reducing however, leavers with less than 2 years of service is still very high, particularly admin and support workers.
-
Guardian of Safe Working report to board
-
FTSU reports to board outlines numbers/themes raised and actions taken and need for more resource to support Guardian. People and Culture Team providing direct support and intervention for Guardian where required including sourcing of additional expertise for escalated concerns.
-
Developing dashboard and metrics to measure leadership development programmes
-
New people and culture indicators agreed (including staff survey, pulse surveys, FTSU) which will be reported to People and Culture Committee. Local accountability assure care group leadership teams at the Quality Performance Meetings alongside the IQPR from January 2024 onwards Internal audit review of Grievance Reporting and Freedom to Speak Up gave reasonable assurance. People & Remuneration Committee tracking all audit recommendations
-
Quarterly pulse surveys feed into dashboard
|
|
|---|---|
Gaps (in controls and assurances)
| Mitigating actions /what more should we do?)
what is required which will inform the Annual Planning Process |
 Var - Fav/(Adv)
Var - Fav/(Adv)



